Background: Lumbar puncture and paracentesis are core competencies in internal medicine, but residents frequently report discomfort performing these procedures unsupervised. Simulation-based training (SBT) has previously been shown to improve resident performance of lumbar punctures on patients, but outcomes after paracentesis SBT have only been assessed on simulators. We hypothesized that SBT would improve internal medicine interns confidence, knowledge and performance of lumbar puncture and paracentesis on patients compared to a control group.
Methods: In the Spring of 2015 and 2016, interns at a large urban academic medical center were randomized to SBT or a control group. The SBT cohort received 4 hours of instruction on ultrasound-guided lumbar puncture and paracentesis task trainers. The session followed an evidenced-based pedagogical framework that included readings and videos prior to the session as well as simulation-based mastery learning. Three months after the training, learners completed a 5-point Likert scale asking if they were comfortable performing the procedure without supervision and/or teaching the procedure to others. They also completed a 10 question multiple choice knowledge assessment created by the author. Both instruments were reviewed by procedure experts and the UCLA Medical Education Research Department for content and response process validation. Following the training, when the interns performed these procedures on patients, their supervisors used a validated global rating scale to rate their performance as novice, beginner, competent, or proficient.
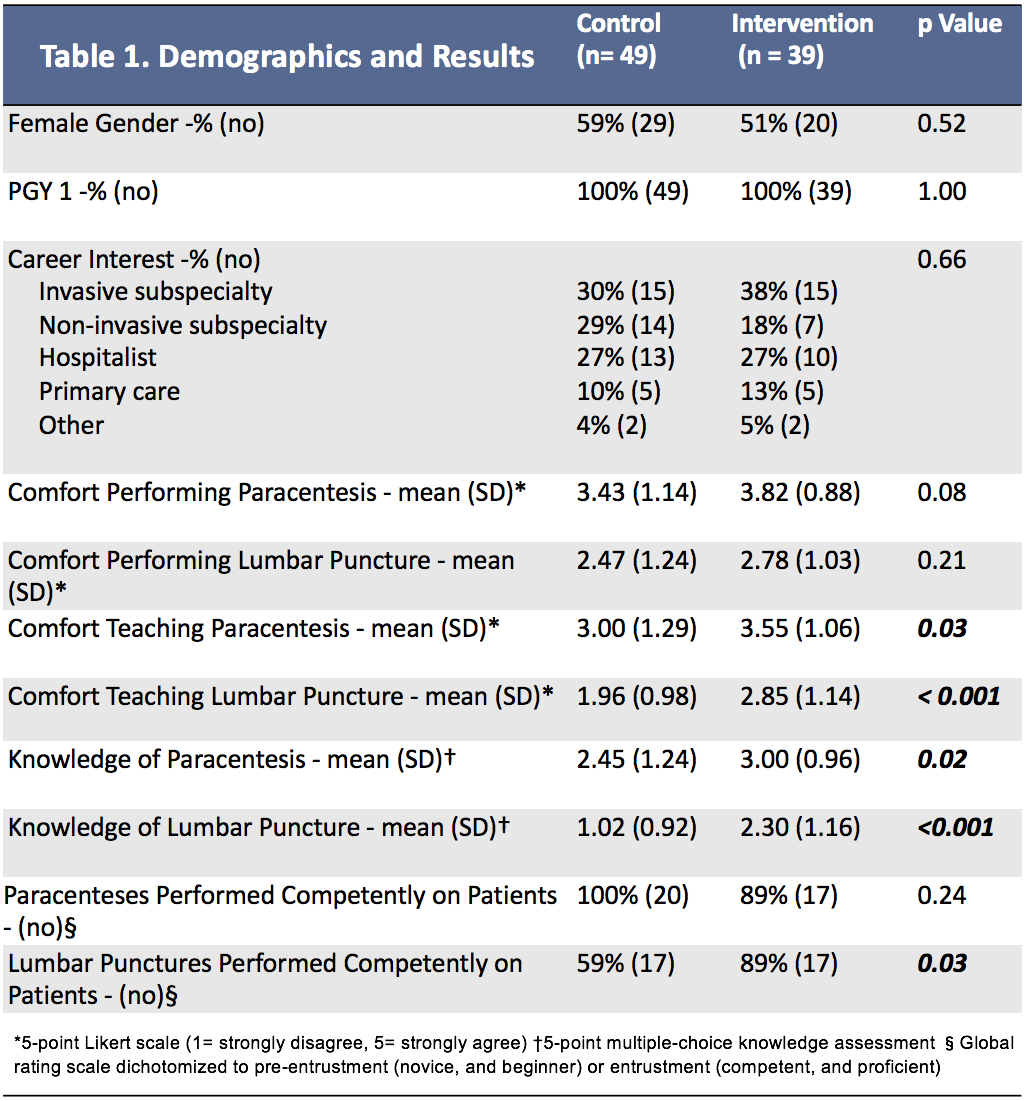
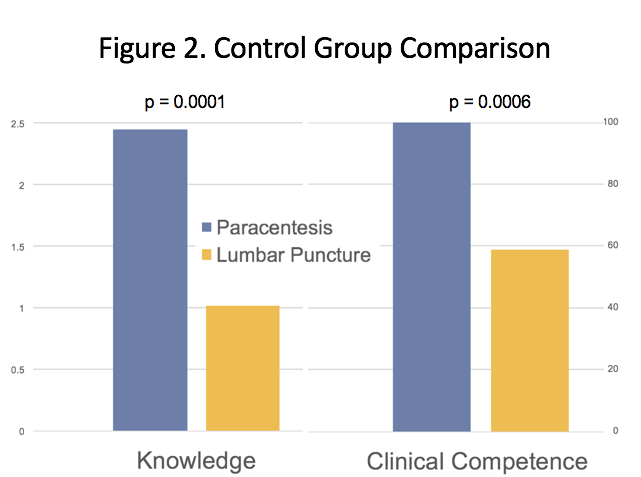
Results: Eighty-eight interns participated in the study, and 39 were randomized to the intervention arm. Baseline demographics were similar between both groups. There was no significant difference in the interns’ confidence in performing a lumbar puncture (2.47 vs 2.78, p = 0.21) or a paracentesis (3.4 vs 3.8, p = 0.09) between the control and intervention groups respectively. The intervention group reported an improved ability to teach lumbar puncture (2.0 vs 2.9, p < 0.001) and paracentesis (3.0 vs 3.6, p = 0.03), as well as an objective improvement in their knowledge of lumbar puncture (1.0 vs 2.3, p < 0.001) and paracentesis (2.5 vs 3.0, p = 0.02). In the year following the SBT, 48 lumbar punctures and 39 paracenteses were performed. More of the lumbar punctures performed by the SBT group were rated as competent or proficient by their supervisors compared to the control group (89% vs 59%, p = 0.03), but no difference was seen in paracentesis performance (89% vs 100%, p = 0.2). When comparing the control groups, interns were more confident, had better knowledge and were more competent performing paracentesis compared to lumbar puncture (p < 0.001).
Conclusions: Though no subjective change in paracentesis and lumbar puncture confidence was found, an objective improvement in the interns’ performance of lumbar punctures on patients was seen after SBT. SBT likely failed to improve performance of paracentesis because of the already high level of competence, confidence and knowledge of this procedure within the control group. Further study is needed to investigate whether this improved knowledge of paracentesis and lumbar puncture results in reduced procedural complications after SBT.