Background: Evidence-based medicine and research are the backdrops to our everyday practice of medicine. Although there are defined steps in carrying research project to publication, there is paucity in the translation of research to practice.(1,2) Over 45% hospitalized patients report poor sleep during their most vulnerable time citing the hospital environment and sleep disruptions from routine care as key factors(3,4). Despite this knowledge, there are few sleep-promoting initiatives in hospitals nationwide. Stemming from the lessons learned from a published peer-reviewed sleep promoting research study (5), we created an outline of translating research into a unit-wide quality improvement initiative.
Purpose: The aim of this sleep-promoting quality improvement initiative was to enhance patient experience during the hospital stay i) by promoting sleep among hospitalized patients ii) reducing provider prescribing patterns during “quiet hours”, and iii) minimizing nursing routine care interventions perceived as sleep disruptions during sleep hours for hospitalized patients. The outline of this quality improvement (QI) initiative was to guide and familiarize clinical hospitalists on basic pathways to operationalized research into clinical programs.
Description: We identified our environment as a 36-bed unit with adult hospitalized patients cared for by hospitalists. We utilized the following six steps in translating a prior research project into a program: Step I: The initial step was to identify the gap in care and hence the problem of interest. We identified poor sleep metrics and frequently cited care disruptions.
Step II: We assembled a multidisciplinary team and key stakeholders that comprised of hospitalists, nurses, patient care technicians and administrators. Using a QI steering committee we defined the scope and outlined the sleep promoting intervention steps feasible for the unit.
Step III: We created a project plan with targeted goals, key metrics and identified timelines for measures that were adapted to the unit-level.
Step IV: We set our targeted metric tools and process measures and defined our outcome measure of success.
Step V: We implemented the project while continually engaging our stakeholders and frontline staff.
Step VI: We evaluated our progress and identified our successes and barriers.
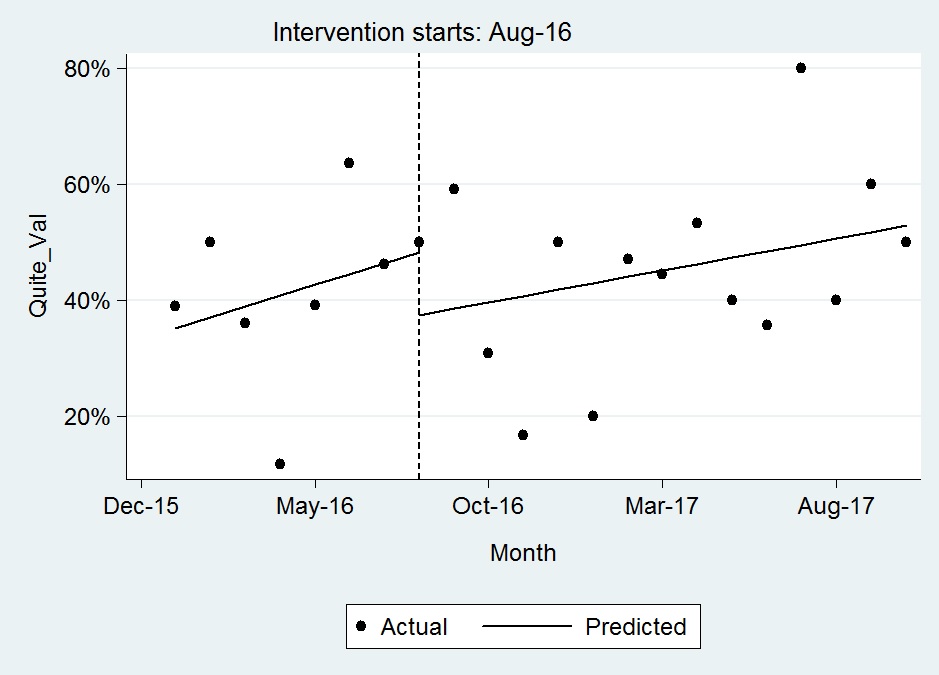
Conclusions: Although clinicians identified sleep as essential for wellness and restoration of patients, few sleep promoting initiatives are practiced as routine care. Hospitalists read about evidence-based research and innovative quality improvement initiatives, however, lack methodology to adapt these to their individual institutions. This sleep promoting QI showed a modest trend towards improvement of Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey metric of ‘quietness at night’ as shown in Fig. 1. The key barrier for modest improvement was semi-private rooms. These steps for translating a research study into a unit-wide intervention were “low effort” and feasible to implement into the routine unit-staff workflow as standard care.