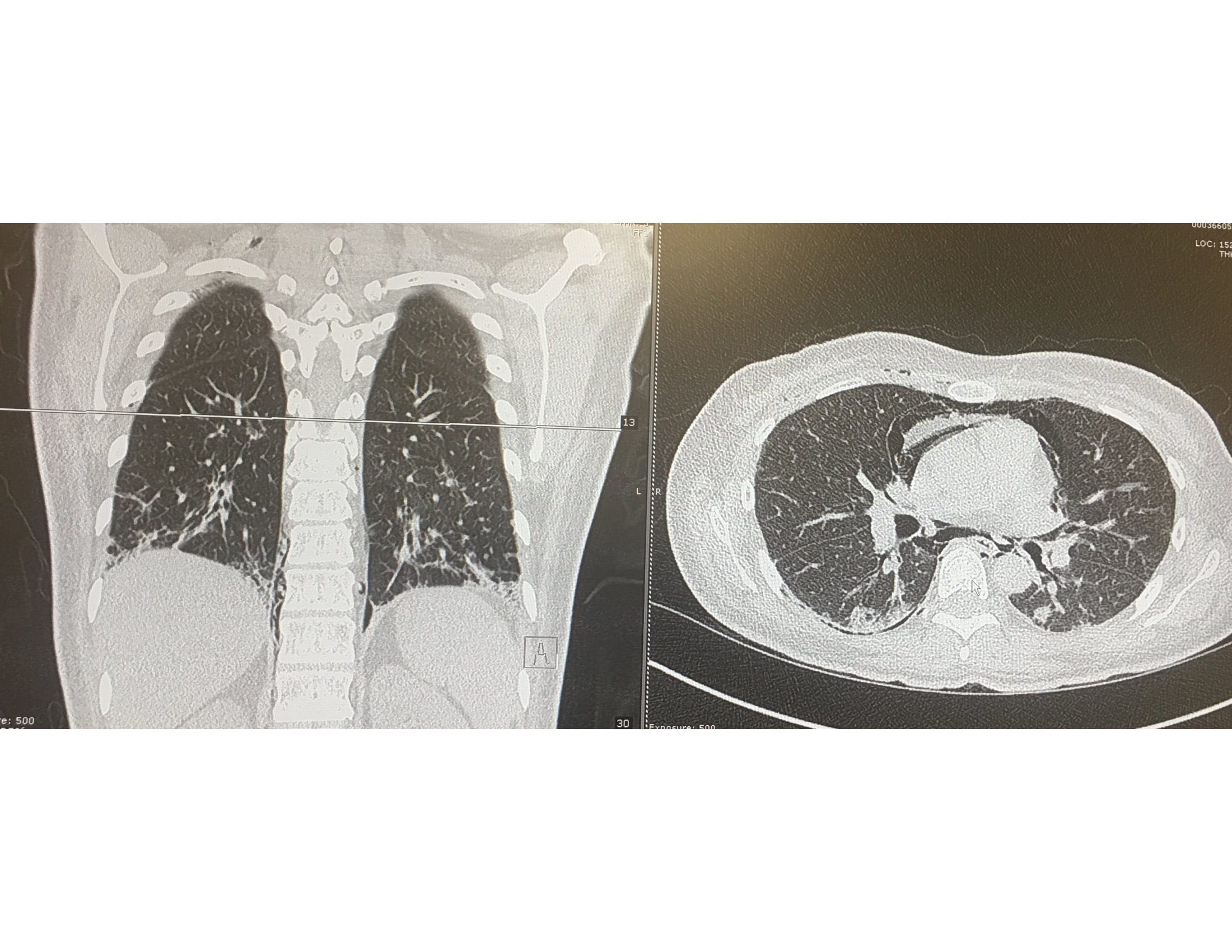
Case Presentation: A 33-year old female presented with 24 hours of subjective fever, severe neck, and chest pain. She was seen 6 months ago for arthralgia of the metacarpophalangeal, proximal interphalangeal and knee joints. Her home medication included Prednisone and Hydroxychloroquine prescribed for Lupus. Her physical examination demonstrated neck crepitus, bilateral crackles, ulcers in the tip of the fingers, erythroderma in elbows, knuckles and eyelids. CT chest revealed pneumomediastinum and right chest wall soft tissue emphysema. There were bilateral pneumothoraces and ground-glass opacities involving lower lobes bilaterally and bibasilar interlobar septal thickening. Laboratory data were significant for normal CPK levels. Anti-Jo1, PL-7, PL-12, Mi2, dsDNA antibodies were negative. ANA ab and Anti mitochondrial M2 were positive. O2 supplementation, Prednisone, Rituximab, and Mycophenolate were given since admission with marked improvement of the symptoms. Upon discharge, she was seen by her rheumatologist who diagnosed Antisynthetase syndrome after new laboratories were ordered.
Discussion: Antisynthetase syndrome is a very uncommon disease, with a reported annual incidence of two new cases per one million adults. This is probably an underestimation caused by a lack of familiarity with this syndrome which criteria were described less than ten years ago. Connor’s criteria include the presence of antibodies against aminoacyl t-RNA synthetase along with features of interstitial lung disease, myositis, Raynaud’s phenomenon, and arthritis. Anti-histidyl antibody (Jo-1) is the most commonly detected antibody (30%).Clinical features of this patient including interstitial lung disease, Goitron papules, mechanical hands, and polyarthritis suggested Antisynthetase syndrome. Imaging studies supported the diagnosis because common findings reported in the literature include ground-glass opacities and interlobar septal thickening as seen in this patient. However, this is a challenging scenario because the patient did not meet diagnostic criteria due to a lack of specific antibodies. This could be explained by autoantibody levels fluctuation depending on disease activity. Also, only a few aminoacyl transfer RNA synthetase antibodies have been identified, many are still not available for laboratory detection.In terms of treatment, there are not clinical trials due to the rarity of this condition. However, cases reported indicating that high dose steroids are the most effective medication in controlling acute pulmonary disease associated with this syndrome. They are used in combination with mycophenolate, and rituximab to improve the prognosis. Complications like spontaneous pneumothorax are managed with oxygen and supportive therapy on stable patients.
Conclusions: Our case report illustrates the challenge that represents the diagnosis and treatment of Antisynthetase syndrome. At the time of the publication, only 8 aminoacyl-tRNA synthetases antibodies out of 20 have been identified which means that many cases will remain undetected until new testing is developed. It is important to create awareness between health care providers because the management of these patients will be very different from other cases of spontaneous pneumothorax and interstitial lung disease seen at the hospital. Steroids, Mycophenolate, and Rituximab should be given early in the management even when a formal diagnosis of anti-synthetase syndrome cannot be done without specific antibodies.