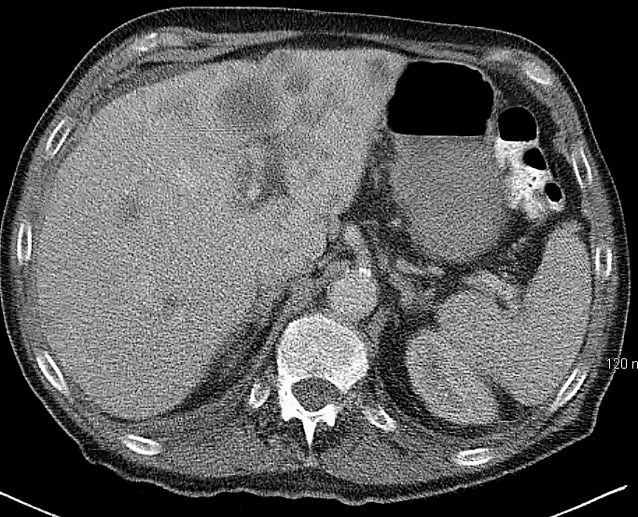
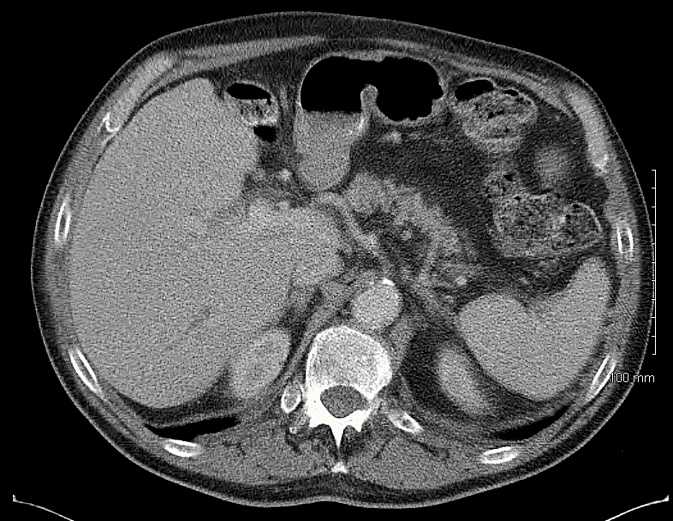
Case Presentation: A 76-year-old man with seropositive RA treated with MTX 15-20mg weekly for at least four years presented to the hospital with worsening fatigue, generalized weakness, poor appetite, and dyspnea. Contrast-enhanced computed tomography of chest abdomen and pelvis (CT CAP) demonstrated numerous pulmonary nodules, centrally hypodense left retroperitoneal soft tissue masses which may represent necrotic retroperitoneal lymph nodes, sclerotic appearance of both femoral heads and right lateral seventh rib, enlarged prostate with mass effect on bladder, and hepatic hypodensities, suggestive of metastatic spread of disease. Histopathological examination of liver mass was consistent with CD10-positive B-cell lymphoma with aggressive features and extensive necrosis. Hospice care was recommended due to his advanced age, functional status, and malignancy. His MTX had been discontinued on hospital admission. Five months later, the patient felt improved and revoked his home hospice, wanting re-evaluation for his diagnosis. Repeat CT CAP in 6 months demonstrated complete resolution of the pulmonary, hepatic, and sclerotic bone lesions without any chemotherapy or radiation treatment.
Discussion: Malignant lymphomas are one of the most common malignancies in the United States. Patients with rheumatoid arthritis have increased risk of malignant lymphoma. Disease activity may be a risk factor for developing lymphoma, but there are also more reports of lymphoma in RA patients treated with MTX. Malignant lymphoma is likely to occur in patients with more than 8-year history of rheumatoid arthritis with total intake of more than 180 mg of MTX. The potential link between RA and lymphoproliferative disorders is supported by studies that show a reduced ability of T cells in a patient with RA to control EBV infection. Persistent or chronic stimulation of the immune system by hepatitis C virus may result in clonal expansion of B-cells in the liver. Patients who have chronic inflammation due to infection with HTLV-1, HIV, Hepatitis C virus, or EBV, also have an increased risk of developing malignant lymphoma. Because of persistently in the B cells to transform these cells, EBV can play a role in lymphomagenesis. Several case reports have suggested a probable oncogenic role of EBV in RA patients with MTX-lymphoproliferative disorders. However, there is no increased distribution of EBV-lymphoma seen in RA patients when compared to lymphomas in general population.In malignant lymphoma rising during treatment with immunosuppressants such as MTX, spontaneous remission can occur after withdrawal of this medication such as in this case. Additionally, it frequently involved extranodal sites such as lung, pancreas, kidney, skin, salivary glands. Based on this case and others in literature, we suggest discontinuation of MTX treatment in any patient diagnosed with or suspected of having lymphoma before initiation of systemic chemotherapy or radiation. However, close initial observation every 4 to 8 weeks for early regrowth of disease even in responding patients is warranted. In cases in which the lymphoma persists, CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) therapy or irradiation may be needed.
Conclusions: Hospitalists should be aware that methotrexate-associated lymphoma may be reversible. Withdrawal of immunosuppressive agents may cause regression or complete resolution of lymphomas.