Background: Identification of pathogens causing community-acquired pneumonia (CAP) in hospitalized patients has improved with the utilization of nasopharyngeal (NP) polymerase chain reaction (PCR). Literature shows that 20-25% of pathogens are identified when using urine antigens, sputum and blood cultures, and can improve up to 70% when adding NP PCR for viruses, Staphylococcus aureus and Streptococcus pneumoniae. Our study compared the Biofire sputum pneumonia film array (PFA) panel to a multitest bundle (MTB). We postulated the number of patients with detectable pathogens could be increased with fewer individual tests by using the recently Food and Drug Administration (FDA) approved PFA multiplex PCR panel.
Methods: Over 2 years, we compared pathogen detection using the PFA vs the MTB in patients admitted from the emergency department with CAP. The PFA probed for the presence of 18 bacterial species and 17 viral targets from sputum. The MTB included: sputum and blood cultures, Streptococcus pneumoniae and Legionella urine antigens, NP respiratory film array panel that identified 17 viruses and 3 atypical bacteria, nasal nucleic acid amplification test (NAAT) for Streptococcus pneumoniae and Staphylococcus aureus. Two serum procalcitonin (PCT) levels were obtained to separate bacteria and viral infections and adjudicate bacterial invasion from colonization.
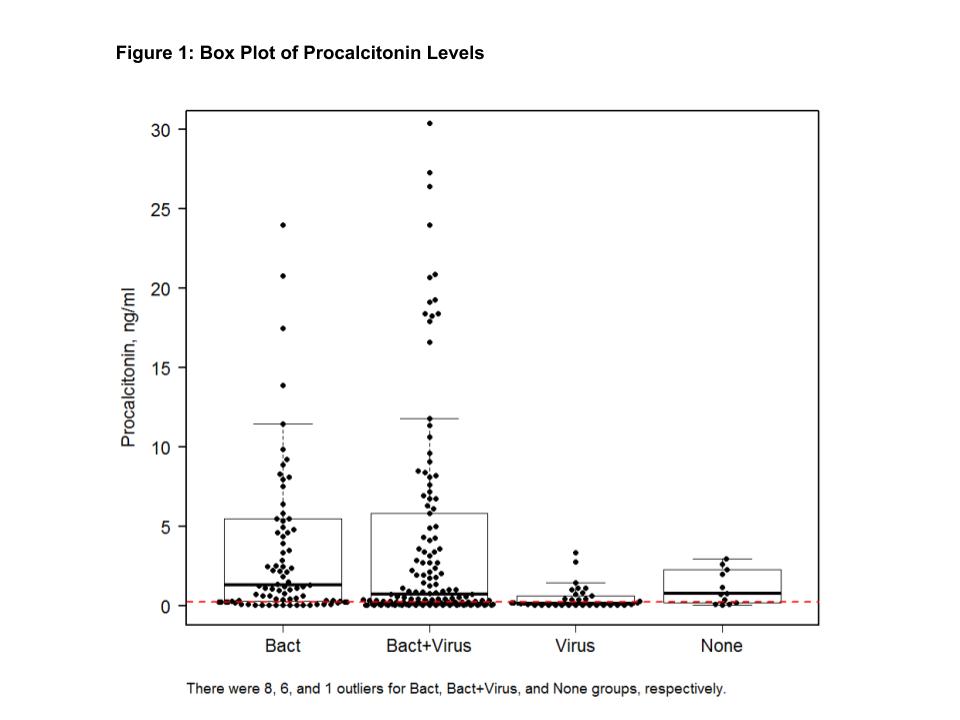
Results: Of 585 enrolled patients, 278 (47.5%) were evaluable and 307 (52.5%) were non evaluable due to alternative diagnoses (50%), inability to produce sputum (45.3%), or incomplete diagnostic work up (4.2%). In the evaluable patients, only virus pathogens were detected in 34 (12.2%) patients; only bacterial pathogens in 90 (32.4%) patients; virus and bacteria were detected in 141 (50.7%) patients. To note, 13 patients (4.7%) had no pathogen detected. One or more potential pathogens were detected in 208 (75.1%) with the PFA vs 182 (65.7%) with the MTB. For example, H. influenzae was detected by PFA in 94 patients and in 22 patients with the MTB, p<0.001. One or more viral pathogens were detected by PFA in 168 patients compared to 112 patients with the MTB, p<0.001. Influenza was detected by PFA in 62 patients and by the MTB in 40 patients, p<0.001.The result of serum PCT levels are in Figure 1. Low PCT values helped separate colonization from invasion in detected bacterial pathogens.The cost of the PFA was calculated at $190 vs $223 for the MTB due to the use of 4 tests with the PFA vs 7 tests with the MTB.
Conclusions: The detection of both potential viral and bacterial pathogens was significantly higher with the PFA compared to the MTB. The expense of the PFA was less than the MTB. Our study showed that using targeted testing and PCT can improve the detection of potential viral and/or bacterial pathogens causing CAP and reduce the number of tests needed for pathogen detection in patients with CAP.