Case Presentation: We present the case of a 42-year-old man in otherwise good health who was admitted to our hospital with several days of fevers, ear pain, hearing changes, and vertigo. The patient initially presented to his primary care provider with several days of subjective fever and left ear pain. Examination revealed edema and erythema of the left pinna and external auditory canal. Treatment was started with amoxicillin-clavulanic acid for presumed cellulitis.He subsequently developed mild tinnitus, positional vertigo, hearing change, and fever, and presented to our emergency department. Examination revealed a new thin, white exudate in the auditory canal. Suspecting progression of cellulitis, the patient was discharged home with oral ciprofloxacin.
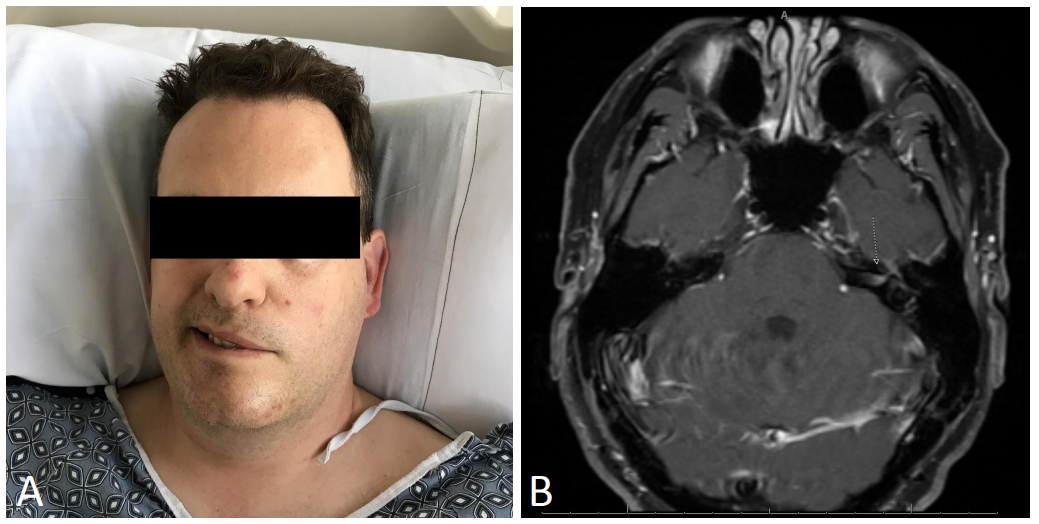
The following morning, he developed left-sided facial paralysis (Figure 1A) as well as a vesicular eruption involving the left external auditory canal (Figure 2), mandible, and nose, prompting referral back to the emergency department. Inpatient examination also noted diminished hearing, bilateral nystagmus, and a positive head impulse test to the left. Treatment was initiated with acyclovir and prednisone, and the patient improved over the subsequent forty-eight hours.
Following discharge, scrapings of the auditory canal lesions tested positive for varicella zoster virus. Magnetic resonance imaging demonstrated abnormal enhancement of the left seventh cranial nerve (Figure 1B). Six weeks after discharge, reported facial strength improved to “85%” of baseline.
Discussion: Initially described in 1907, Ramsay Hunt Syndrome represents the second most common cause of non-traumatic facial weakness, accounting for up to 7 percent of facial palsies overall. Defined as a unilateral facial palsy associated with vesicular eruption of the external auditory canal, it is caused by a reactivation of latent varicella zoster virus in the geniculate ganglion of the facial nerve. Other features may include retro-auricular pain, tinnitus, hearing change, or vertigo. Although early treatment has been associated with improved outcomes, diagnosis may be delayed by late onset of rash or lack of recognition of the syndrome.
We highlight a case of Ramsay Hunt syndrome with an atypical initial presentation, which complicated diagnosis and delayed treatment.
Although vesicular rash is considered a defining feature of this syndrome, onset may be late in the disease course. Moreover, as many as 2–8% of cases will never develop a rash (termed zoster sine herpete). Accordingly, recognizing auricular pain, hearing change, nystagmus, or vestibular findings as symptoms of this disease may facilitate early diagnosis.
Conclusions: Left untreated, Ramsay Hunt syndrome can lead to residual facial paralysis, hyperacusis, vertigo, and dysgeusia. Fortunately, early treatment has been associated with better outcomes. Consequently, maintaining a high index of suspicion in concerning clinical presentations can better direct the physical examination and laboratory testing of affected patients, and may limit long-term morbidity from this condition.