Background: As hospital systems look to a future of accelerated movement toward value, hospitalist engagement will be necessary for identifying opportunities and executing improvement in the inpatient space. Improvement in efficiency of clinical care, and related decrease in length of stay (LoS), has been identified as a way hospitalist teams can contribute to value-based care. Many barriers to improvement in LoS are outside of the clinical care team’s control and can leave hospitalists feeling powerless to contribute. Hospitalists can assist in identification of these non-clinical barriers for intervention by the appropriate team.
Purpose: Here we describe the experience of a large hospitalist team within an academic medical center of improving hospitalist value contribution through reduction inpatient LoS while simultaneously improving team satisfaction between October 2021 and October 2023.
Description: The following initiatives were designed to improve the environment for hospitalist engagement in value work and improve efficiency of care: • Survey hospitalists team for opportunity o Provided needed information about clinical and nonclinical opportunities and allowed targeted data review • Obtain performance data o Development of individual and team Epic Dashboards to track metricso Use of Vizient to compare to like organizations by diagnosis o Monthly evaluation of opportunity days (days over GMLOS) by DRG with focus on patients discharging home without services – to identify clinical opportunity • Provide mode of communication and opportunity for physicians to raise barriers and request real time intervention o Discharge delays tool use in Epico Appropriate teams assuming responsibility to eliminate barrier • Optimize hospitalist workload o 15-16 patient assignments supported by implementation of back up call system • Increase geographic cohorting to allow for participation in interdisciplinary rounds o Dissociation of rounding and admitting assignments o Engagement of clerical team to improve cohorted assignments, collect and follow data • Frequent updates about progress o Monthly team meetings, weekly newsletters to celebrate success and provide education• Leadership driven improvement work o Hospitalist Division Chief became Physician Leadership for system LoS Program o Targeted collaboration for clinical opportunities with other service lines o Development and staffing of remote patient monitoring program for transitional careo Engaging Clinical Standardization team to support clinical pathway creation o Advocacy for system wellness support• Leadership support for team members engaging with interest in initiative developmento Physician funding for sickle cell disease program development, resource allocation for hospitalist procedure team
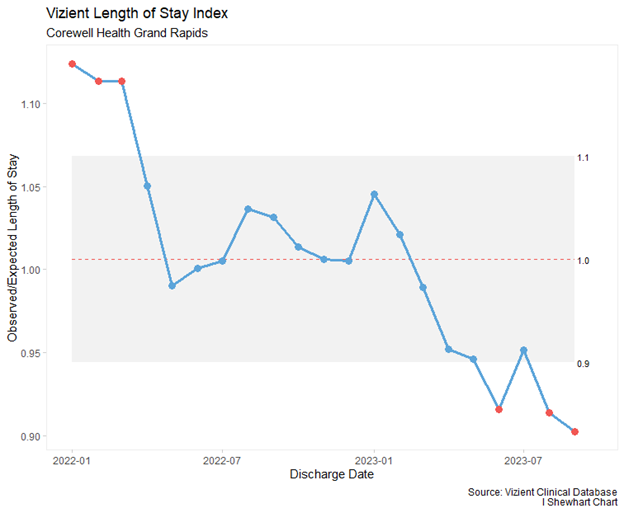
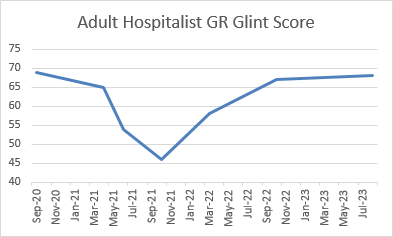
Conclusions: These strategies contributed to an improvement in LoS Index (Vizient AMC Cohort) from worse than median in 2022 to top decile in 2023. Hospitalist LoS peaked January 2021 at 8.32 days and improved to 5.71 days by September 2023.Team satisfaction via system survey demonstrated a 20-pt improvement between Fall of 2021 and 2022 which sustained into 2023. Satisfaction score based on composite of two questions; overall job satisfaction and likelihood to recommend employer. Team engagement in initiatives that improved efficiency, decreased LoS, and increased team satisfaction improved – despite continued need for locum physicians and multiple years of flat hospitalist compensation benchmarking.