Background: Effective doctor-patient communication is crucial for the exchange of important information. Improved communication can positively influence patient satisfaction, adherence and ultimately can lead to improvement in health outcomes.Patient satisfaction scores in the inpatient setting are elicited using the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. Effective communication between a physician and a patient is crucial to nurture a therapeutic connection and patients appreciate doctors who engage through active listening and explanations of clear treatment strategies.
Purpose: The Agency for Healthcare Research and Quality advocates that improving patient experience has inherent value to patients and families and is therefore an important outcome. Patients’ experiences with care, particularly around communication with physicians correlate with adherence to medical advice and treatment plans.
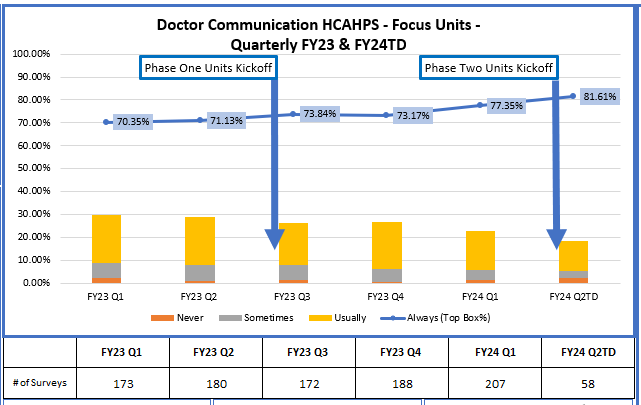
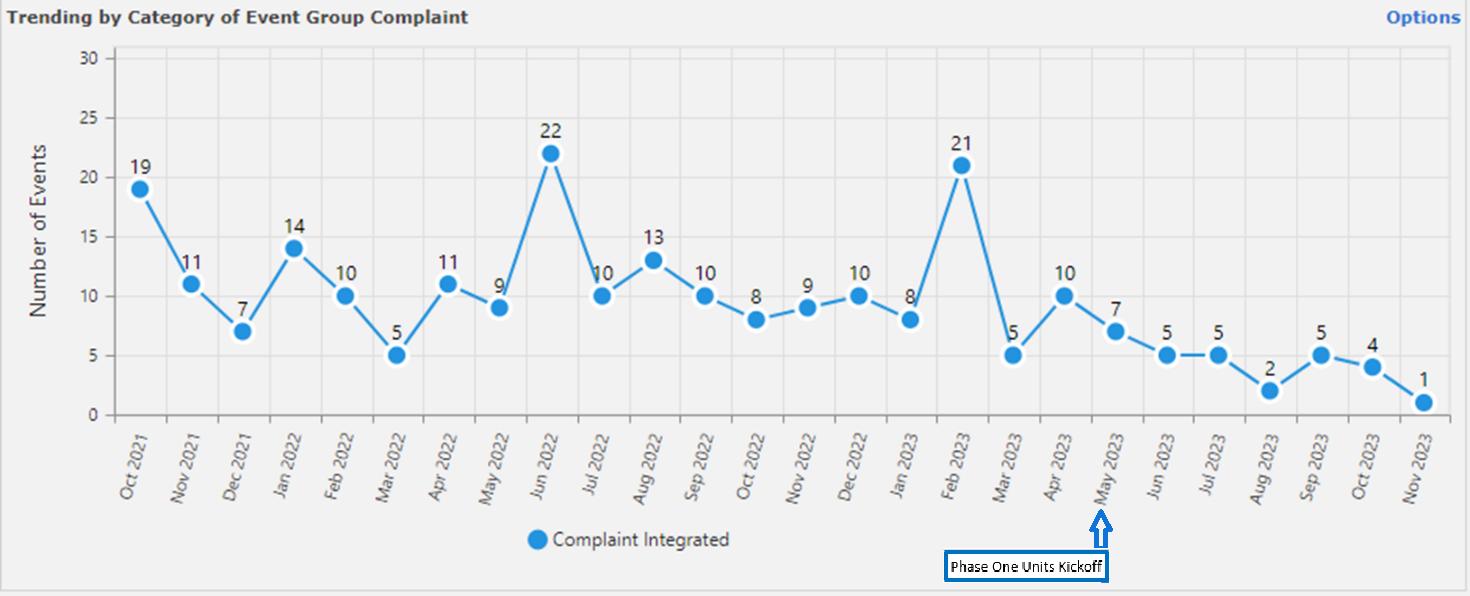
Description: We formed a multidisciplinary group of physicians, nurses, case managers, and patient experience specialists. The committee analyzed HCAHPS scores and comments for nursing units and physician services and reviewed literature for best practices with a goal to implement interdisciplinary rounds. The Committee selected the format of “TEMP – Interdisciplinary rounds (IDR) “12 The aim of this project is to improve patient experience as measured by the HCAHPS Doctor Communication top box scores through implementation of beside TEMP-IDR. TEMP IDR creates an efficient microsystem on each floor to link daily care processes and create a shared information environment. The team includes the patient and their family, the attending physician, the bedside nurse, the case manager, and charge nurse or clinical leader. A script was created for each discipline for timely and effective communication. Rounds started on a specific time every day with an average of three to five minutes spent with each patient. In Phase I, TEMP-IDR was implemented on four hospitalist nursing units. The hospitalists were given educational talks on the TEMP IDR process and Doctor Communication Best Practices. Weekly Nursing Unit Huddles were created to promote the use of the TEMP mnemonic sheet by nurses. We built in Quality Assurance through Physician Leader rounding where we gathered feedback from patients, frontline team members, and leaders to understand successes and barriers. We implemented improvements through weekly update emails and bi-weekly committee meetings. TEMP IDR was expanded to three more medical-surgical units after three months as Phase ll.
Conclusions: Our data for the first 6 months shows that the Hospitalist physician services and focus units that implemented TEMP IDR show an improvement in the HCAHPS Doctor Communication Domain Top Box Scores. There has also been a significant decrease in the number of patient complaints. Physicians have anecdotally reported a substantial decrease in the secure chat messages between the nurses and the physicians. Our initial data shows that implementation of TEMP-IDR can improve patient experience and decrease patient complaints. The main contributors to the success of this project were the use of a standardized script and weekly huddles. The barriers to the implementation of the IDR were the change in work pattern and continuity of care. Our plan is to continue to roll out TEMP-IDR to additional unit as we continue to improve the process with feedback from patients and all involved disciplines.