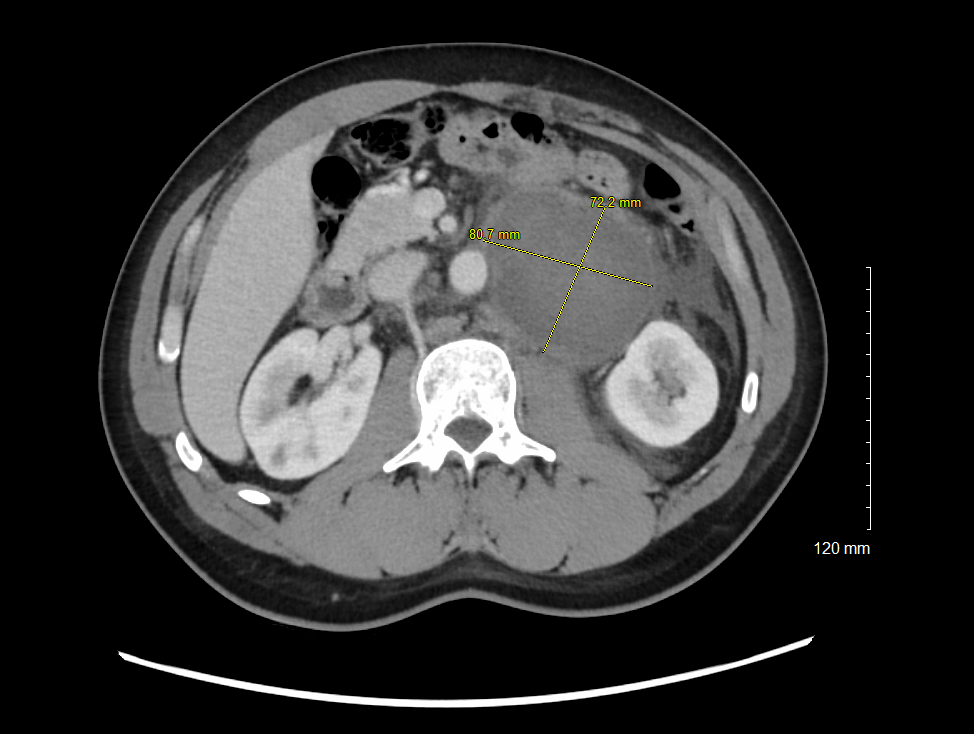
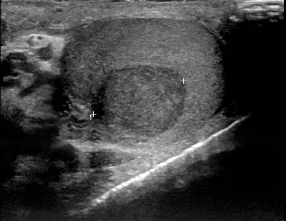
Case Presentation: A 40-year-old male presented with acute-onset left back and flank pain radiating to the lower abdomen, along with nausea and vomiting. His initial presentation was most concerning for nephrolithiasis and CT Abdomen/Pelvis was obtained. Imaging demonstrated bulky retroperitoneal lymphadenopathy with a large paraaortic conglomerate, measuring up to 14cm in diameter. The mass was compressing the left GU system, causing mild hydronephrosis of the left kidney, which is likely the etiology of his presenting symptoms. Additional imaging findings included gynecomastia and splenomegaly, raising concern for lymphoma vs. metastatic disease. CT-guided biopsy of the retroperitoneal lymph nodes was scheduled, and the patient was admitted for further workup. Extensive chart review revealed the patient had a history of a left varicocele in the early 2000’s and concern for infertility in 2017. The patient also endorsed intermittent swelling and asymmetry of his left testicle for the past several years, raising suspicion for testicular cancer. Laboratory studies were notable for an elevated beta hCG and LDH, with AFP within normal limits. Urology indicated the patient’s clinical and lab findings were most concerning for seminoma. They advised against retroperitoneal biopsy due to the high risk of seminoma seeding the biopsy tract and recommended proceeding with an orchiectomy. The orchiectomy pathology report demonstrated pure seminoma limited to the left testes, with the largest diameter being 4.4cm. CT chest and MRI brain were also completed, which ruled out pulmonary, mediastinal, and cranial metastases. The patient was ultimately transferred to the oncology service and began chemotherapy with bleomycin, etoposide and cisplatin (BEP) with the plan to complete 3-4 cycles as per NCCN guidelines. Staging of this patient’s testicular cancer is incomplete at this time, as post-orchiectomy beta HCG and LDH values are required to determine the final stage.
Discussion: Patients first presenting with retroperitoneal lymphadenopathy may pose a diagnostic challenge to providers, particularly if the patient’s initial presentation does not include signs and symptoms of a primary neoplasm. Retroperitoneal lymphadenopathy may mistakenly masquerade as lymphoma, particularly if splenomegaly is also present. If metastatic disease is at all suspected, patients should be thoroughly evaluated for a primary lesion prior to biopsy of the retroperitoneal lymph nodes.
Conclusions: In males presenting with retroperitoneal lymphadenopathy, clinicians should consider metastatic testicular cancer as a possible diagnosis; if seminoma is suspected, care should be taken to avoid FNA biopsy of the retroperitoneum or primary malignancy, due to the high tendency of seminoma to seed biopsy tracts.