Background: The designation of a patient as outpatient versus inpatient status at time of discharge affects how hospitals bill Medicare for services because the center for Medicaid and Medicare services (CMS) reimburses hospitals at a higher rate for inpatient when compared to outpatient designation(1). Since the fiscal year of 2014, one of the major benchmarks for outpatient status as defined by CMS was that the expected patient stay was less than 48 hours with a few exceptions such as certain procedures listed by CMS(1). To discourage hospitals from designating patients as inpatient when not appropriate, CMS established the recovery audit program in 2003 to identify and correct past improper payments to hospitals(1) . At Stanford hospital, case managers are supposed to review each patient’s designation prior to discharge for compliance with CMS criteria for inpatient stay. When this safety net fails, Stanford hospital does not bill Medicare for patients who erroneously designated as inpatient. These write-offs as they are called leads to a significant loss of income to Stanford hospital on a yearly basis.
Methods: A best practice alert (BPA) intervention was developed and could fire upon signing of discharge order for Medicare patients who have the designation of inpatient but have stayed less than two midnights provided they were in an acute level of care. Upon firing, the primary team would be asked to confer with the case manager who also gets a message to review the patient’s designation as inpatient. All patients that were admitted between July 18, 2019 and October 2019 at Stanford hospital were randomized to the intervention arm (BPA fires) or control (BPA is silent). Chart review was then conducted and information regarding patient’s designation either as inpatient vs outpatient at time of discharge, case manager notes regarding whether inpatient designation was appropriate and BPA override reason in cases where a patient was not converted from inpatient to outpatient was documented. Estimated number of write offs was calculated in the intervention arm using the number of patients that were not converted from inpatient to observation as a surrogate followed by deduction of those who met criteria for inpatient stay after case manager review. Similar calculation was done for the control arm but since not all patients were reviewed by case manager because of lack of BPA reminder, the number of patients who would have met criteria for inpatient stay was estimated using the intervention arm as a surrogate.
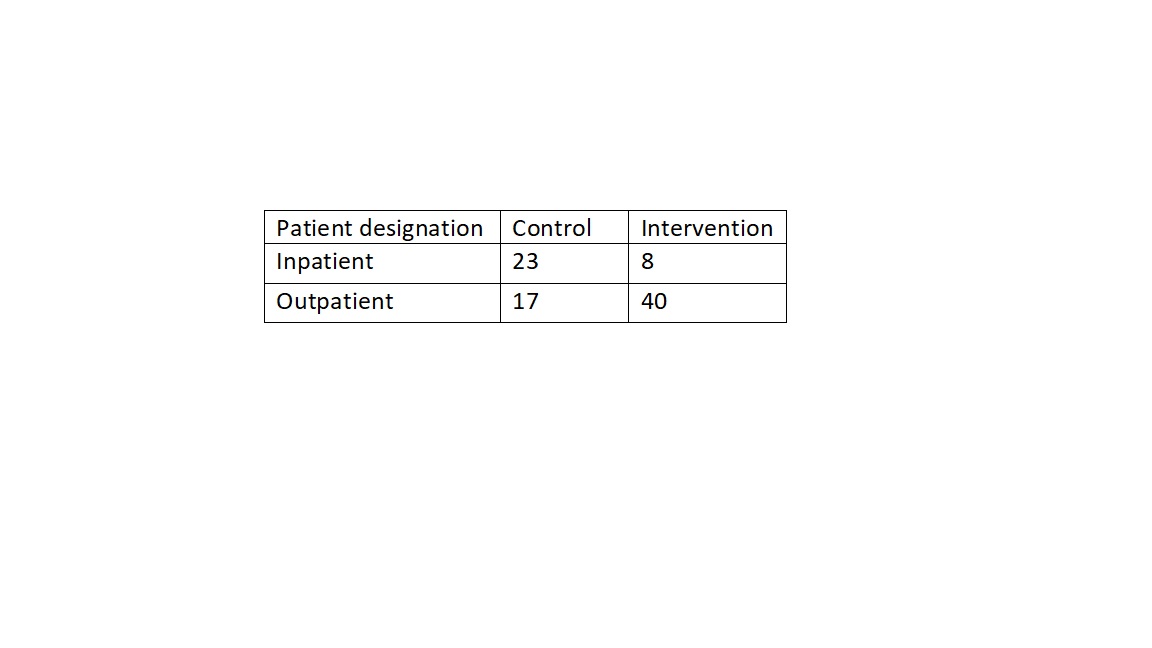
Results: There were 88 patients in this study; 40 in the control arm and 48 in the intervention arm. In the intervention arm, 40 were converted to outpatient status after case manager review of the patient’s designation. 7 out of the 8 patients who were not converted were deemed to have met criteria for inpatient stay by our case manager leading to an estimated Medicare write off of 1. There were 40 patients in the control arm of which 23 were designated as inpatient at time of discharge for an estimated number of write offs of 17.
Conclusions: Using a best practice alert to remind the primary team and case manager to review patient’s designation to ensure appropriate classification as inpatient or outpatient, we were to reduce the estimated number of write offs from 17 to 1 which amounts to 2.4 million dollars in potential savings to Stanford hospital.