Background:
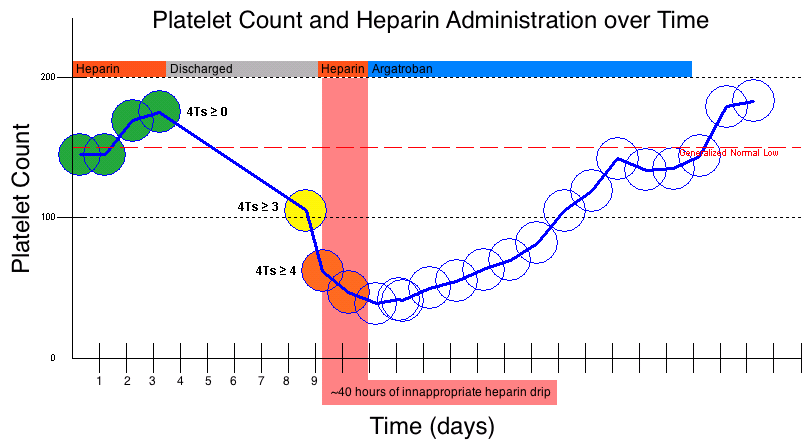
Heparin-Induced Thrombocytopenia (HIT) is a rare (0.1-1% of heparinized medical patients) but devastating (up to 10% mortality) side-effect of heparin administration[1]. In thrombocytopenic patients, the pre-test probability of HIT is estimated by the validated “4Ts Score”, which is used to risk-stratify patients into Low (0-3 points), Intermediate (4-5 points), and High (6-8 points) likelihoods of HIT and inform the decision of whether to stop heparin and pursue further workup. This project describes a decision-support algorithm that incorporates the two calculable components of the “4Ts Score”—Thrombocytopenia and Timing—to create an “Automated 2Ts Score” with the intent of preventing delayed diagnosis of HIT.
Methods:
The “Automated 2Ts Score” decision-support algorithm was prototyped using Virginia Mason’s Clinical Data Warehouse, a searchable database of lab results and medication administrations. For every platelet count posted within 14 days of the initial administration of a heparin product, an “Automated 2Ts Score” was calculated. If the total point value was 4, the pre-test probability of HIT was estimated as “at least intermediate”, necessitating further evaluation by the treating physician. The algorithm was retrospectively performed on all heparinized thrombocytopenic patients seen at Virginia Mason Medical Center between April 2014—April 2015 (N=23,696).
Results:
Of the 23,696 heparinized patients evaluated, 298 had an “Automated 2Ts Score” of 4, corresponding to a “4Ts Score” of at least 4 and, thus, a pre-test probability of HIT at least 14%[2]. Of these 298 algorithmically-identified patients, only 60 underwent subsequent workup with a HIT antibody test. Of these 60 patients who underwent further workup, the mean delay from the Intermediate “Automated 2Ts Score” to the HIT antibody test order was 23.4 hours. For the 4 patients subsequently found to have HIT after initial algorithmic identification, 13 additional doses of heparin were administered.
Conclusions:
Computer systems running clinically-validated algorithms can supplement the care provided by physicians and prevent diagnostic delay in conditions with objective, algorithmically-identifiable features. Additionally, the use of a clinical data warehouse enables rapid prototyping and retrospective application of potential interventions, facilitating the use of the Plan-Do-Study-Act (PDSA) cycle in developing healthcare quality innovations. Further work will incorporate this “Automated 2Ts Score” into the EMR, enabling physicians to benefit from its real-time assessment of HIT risk.
Figures:
Figure 1: An example in which an Intermediate-risk 4Ts score was detected algorithmically about 40 hours before it was detected clinically.
References:
1. Linkins Lori-Ann A., Dans Antonio L., Moores Lisa K., et al. Treatment and prevention of heparin-induced thrombocytopenia: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141.
2. Lo G. K., Juhl D., Warkentin T. E., Sigouin C. S., Eichler P., Greinacher A.. Evaluation of pretest clinical score (4 T’s) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. Journal of Thrombosis and Haemostasis. 2006;4:759-765.