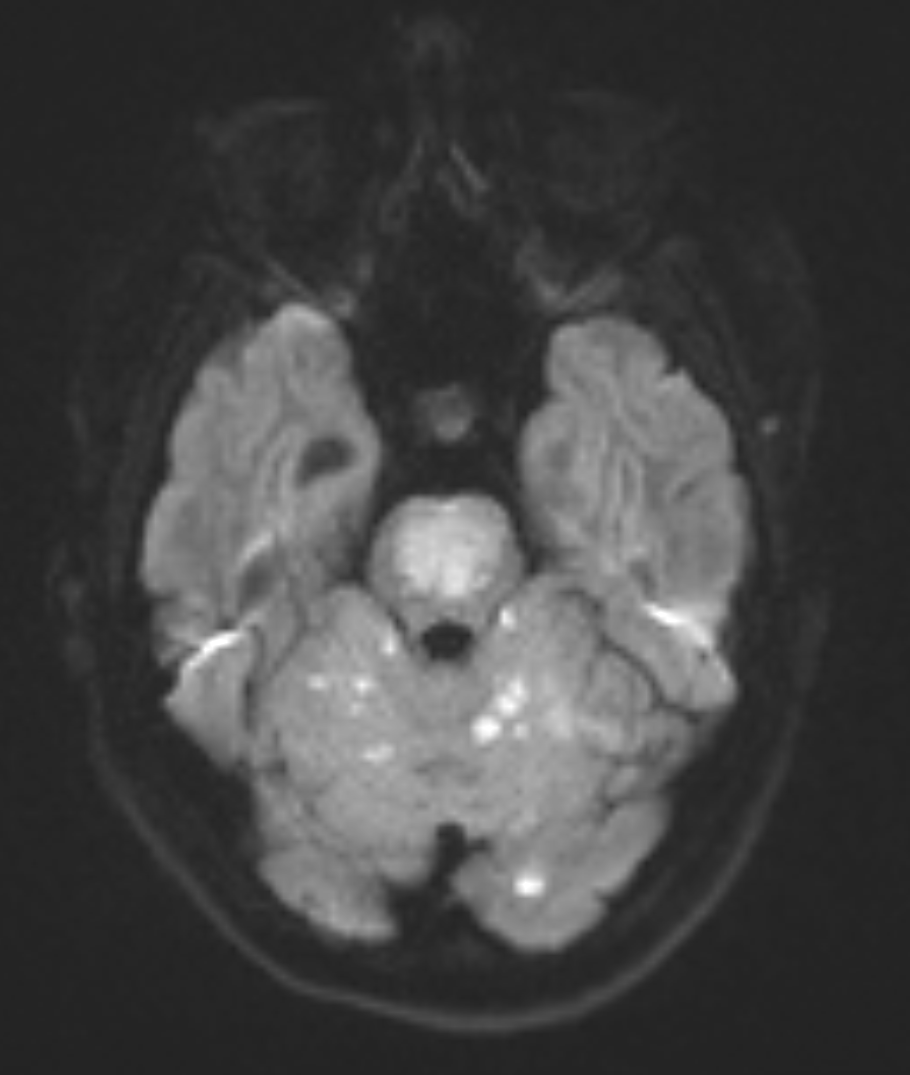
Case Presentation: A 19-year-old woman with a history of polysubstance abuse and recent e-cigarette/vaping product use associated lung injury (EVALI) presented to the Emergency Room (ER) at a rural medical center with Acute Respiratory Failure and Altered Mental Status (AMS). Pt was 3 months post-partum. Past medical history included chronic migraine headaches and Grave’s disease. Her initial neurological condition warranted bag-mask ventilation and immediate intubation upon arrival to the ER. The stat CT scan of the head appeared to be unremarkable. Toxicology screen was positive for cannabis and benzodiazepines. Per her family, the patient continued to use e-cigarettes/vaping products. A few hours into her admission to the Intensive Care Unit, she was noted to have decerebrate posturing and myoclonus of bilateral ankles. The State Poison Control Department and eICU were consulted. EVALI was the initial admitting diagnosis causing the Acute Respiratory Failure, but a CT chest angiogram showed only bilateral atelectasis, no pulmonary emboli. MRI/MRA of the brain demonstrated occlusion of the basilar artery resulting in bilateral acute infarcts in the cerebral hemispheres and pons extending up into the left midbrain, and thalami that were most likely embolic in nature. Her NIHSS score was 25, she was outside the window for tPA. IV Heparin and Coumadin were initiated. Off sedation, the patient was noted to be in spastic quadriparesis with inability to articulate speech, but with preserved self-awareness. A diagnosis of Locked-In-Syndrome (incomplete form) was made as she was only able to move her eyes and blink to communicate yes/no. She was subsequently extubated, had a percutaneous tracheostomy and a PEG tube placement. Pt remains quadriparetic, but is able to move her head now. She communicates by pointing to letters with a laser light on her head. Her power is 2/5 in left upper extremity and 1/5 in all the remaining extremities. Placement in a Long Term Acute Care Facility (LTAC) is anticipated.
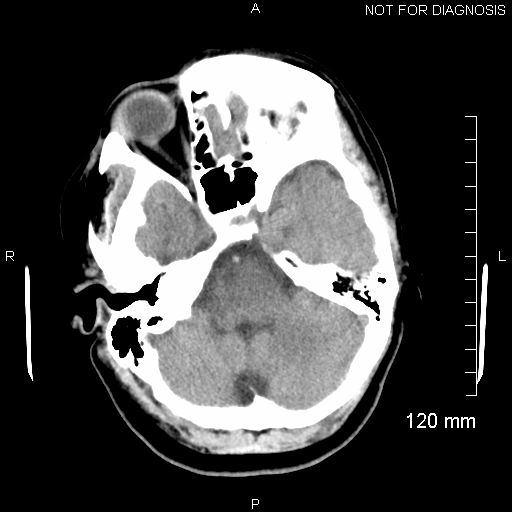
Discussion: Our case highlights the rare clinical diagnosis of the incomplete form of Locked-In Syndrome (first described by the Austrian Neurologist Bauer in 1979). It also reflects Anchoring Bias on the part of the physicians in that they were all initially focused on the history of EVALI causing the Acute Respiratory Failure, when in fact, she was having an acute embolic stroke. There was the presumption that her AMS and abnormal movements were from polysubstance abuse and anoxic brain injury until the MRI/MRA confirmed a posterior circulation stroke. Although the initial stat CT head was reported as unremarkable, on retrospective review of the images, we were able to identify the Hyperdense Basilar Artery Sign (HDBA). The rarity of the Locked-In-Syndrome coupled with the variability of the clinical features on acute presentation proved to be a diagnostic pitfall for the entire medical team.
Conclusions: Conclusion:A high index of suspicion is needed to make the diagnosis of Locked-In-Syndrome on initial presentation, especially in younger patients. The Hyperdense Basilar Artery Sign (HDBA) on non-contrast CT imaging is one of the earliest predictors of a posterior circulation stroke and provides a vital clue towards a diagnosis of basilar artery occlusion. Medical providers should also be aware of the Anchoring Effect (a cognitive bias that causes people to rely too heavily on the first piece of information they receive as a point of reference) which can be associated with diagnostic inaccuracies or suboptimal patient management.