Background: Transition home after hospitalization carries significant risk of adverse patient events, readmissions and increased costs. Despite significant organizational efforts to improve care transitions, there continue to be challenges in implementing consistent interventions that impact key metrics of patient experience with the care transition and 30-day readmission rates.
Purpose: Designing patient-centered systems which improve collaboration between inpatient providers, outpatient providers and patients is imperative to improve care transitions. We developed a patient-focused quality collaborative with hospitals, physician organizations (POs) and patients to innovate the transition processes across the state of Michigan and allow organizations to share the lessons they learn with each other through this initiative. Furthermore, we used innovative improvement methods that incorporated integrated design tools with the creation of institution specific patient journey timelines to better identify local gaps in care transitions.
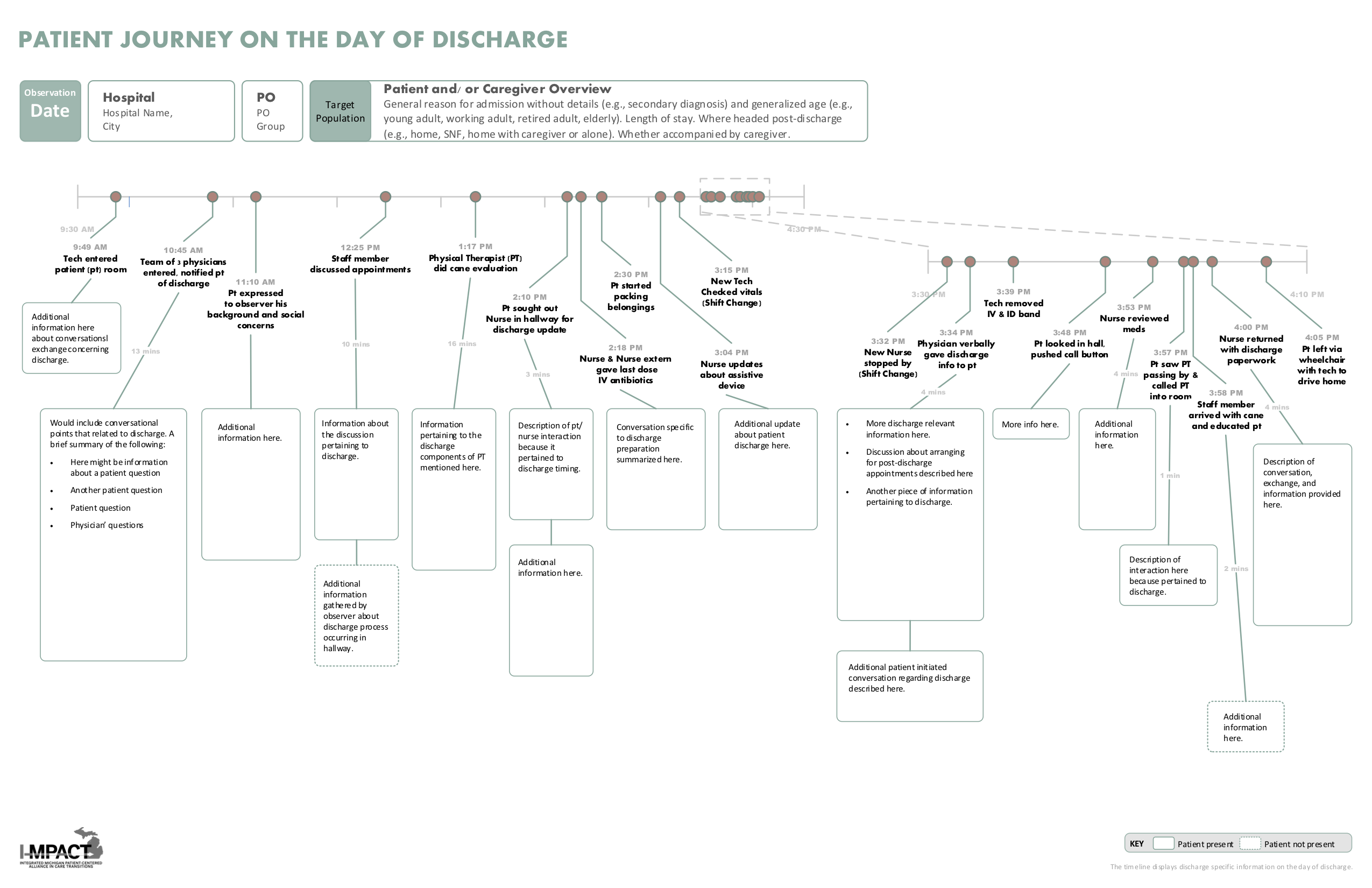
Description: I-MPACT is comprised of clusters, each made up of representatives from a hospital, PO(s)and two patient/caregiver advisors. Each cluster has selected to focus on one of five common disease populations by choosing to target patients who have pneumonia, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), acute myocardial infarct or patients discharged to a skilled nursing facility (SNF). Patients from the target population discharged from cluster hospitals were closely observed in the hours prior to discharge and an innovative patient journey timeline was generated (image 1) using the integrative design process. This novel patient journey timeline was used to focus team discussions and help clusters identify fundamental gaps that occur in the local transition process. Every cluster then developed two unique interventions to improve the discharge process for their selected target population. Lessons learned at individual clusters have been helpful for other clusters and are actively shared on monthly conference calls and at collaborative wide meetings.
Conclusions: We have developed an innovative patient journey map to help identity hospital-specific improvement opportunities at the time of hospital discharge and we used these patient journey timelines to develop 40 unique interventions at 20 different I-MPACT cluster hospitals in a collaborative effort to improve care transitions throughout Michigan. Each of the 20 I-MPACT clusters are actively abstracting data surrounding patient experience at the time of discharge as well as readmission rates and we are building a robust data registry to evaluate the quality of care transitions in our state. We hope the care transition improvement interventions generated from our novel patient journey timelines will positively influence these factors.