Background: With over 50% of hospitalists affected by burnout cited in the literature, it is imperative to evaluate tools and techniques to abate the downstream consequences. Recent work on resiliency has focused on how to decrease emotional exhaustion through exercises that can reframe a negative outlook into a positive perspective. Employing the “three good things” strategy has had evidenced based success for the individual, but this strategy rests on the fact that the individual has to be engaged enough to participate. Physicians affected by burnout may already be too disconnected to utilize an individual stress management technique.
Purpose: To determine if a shared approach to resiliency would decrease collective burnout in a hospitalist group.
Description: According to the Maslach Burnout Inventory Manual, burnout is a syndrome of depersonalization, emotional exhaustion and a sense of low personal accomplishment. It is from this manual that the validated Maslach Burnout Inventory (MBI) questionnaire has been extracted and applied to measuring levels of burnout.
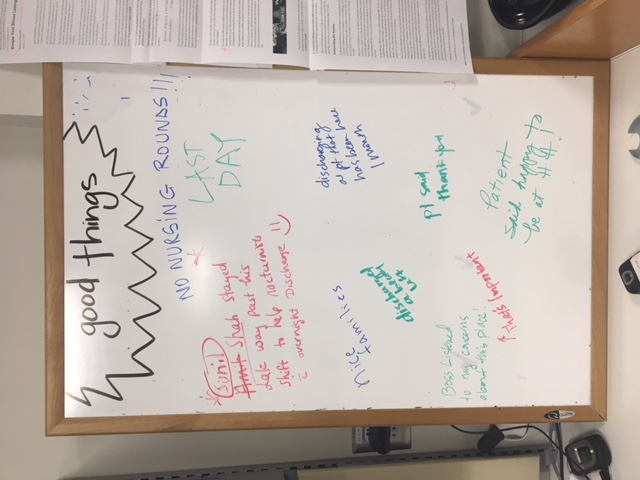
A modified ten question survey based on the MBI was given to our hospitalist group prior to the institution of our resiliency project to establish a baseline understanding of burnout for our practice. Using “Three Good Things” as a framework, we developed a team based strategy to attempt to affect collective resilience. A positivity board was placed centrally in the hospitalist office. Team members were encouraged to write comments and experiences that highlighted any positive part of the day for a two week period. Regardless of participation, physicians were exposed the board throughout their work day. At the end of the two week interval, the same survey was repeated to evaluate collective change, irrespective of contribution to the board.
The comparison of the pre and post surveys yielded two interesting findings. 33% of respondents to the initial survey reported feeling emotionally drained at work every day, while only 16% of respondents reported feeling emotionally drained every day after exposure to the positivity board. Additionally, 33% of hospitalists surveyed felt energetic a few times per week prior to the project, and 50% felt energetic a few times per week after exposure to the positivity board. (It is important to note no hospitalists felt energetic every day before or after the board.) These findings may be skewed by having more responses to the post intervention survey, but the expanded participation of the later survey may possibly be related to increased engagement as a secondary result of the project.
Conclusions: A simple, no cost intervention has the potential to impact perception of a hospitalist team. Utilization of a shared positivity board has the ability to affect facets of burnout irrespective of individual participation. This project shows that emotional exhaustion and energy levels can be influenced by group resiliency techniques.