Background: Anemia is a risk factor for cognitive impairment as a result of the reduced delivery of oxygen to the brain from low hemoglobin (Hb) levels. In ambulatory patients even mild anemia (Hb < 12g/dL) has been associated with reductions in patients’ cognitive function. However, in hospitalized patients it is standard of care to maintain Hb levels far lower, around 7g/dL, as a result of restrictive transfusion practices. This raises the possibility that the lower Hb levels tolerated in hospitalized patients as a result of restrictive transfusion practices, may have a deleterious effect on patients’ cognitive function. This is important because reduced cognitive function negatively effects patients’ self-efficacy and functioning, can increase the risk of delirium and length of stay, and may ultimately impact discharge destination and recovery after hospital discharge. While transfusion trials in hospitalized patients have shown no difference in outcomes between restrictive vs. liberal transfusion thresholds, these RCTs did not examine the effect that lower Hb levels may have on patient’s cognitive function. As such, they cannot answer whether lower Hb levels during hospitalization may effect cognitive functioning. Therefore, the purpose of this study was to test for an association between Hb levels during hospitalization and patient’s cognitive function.
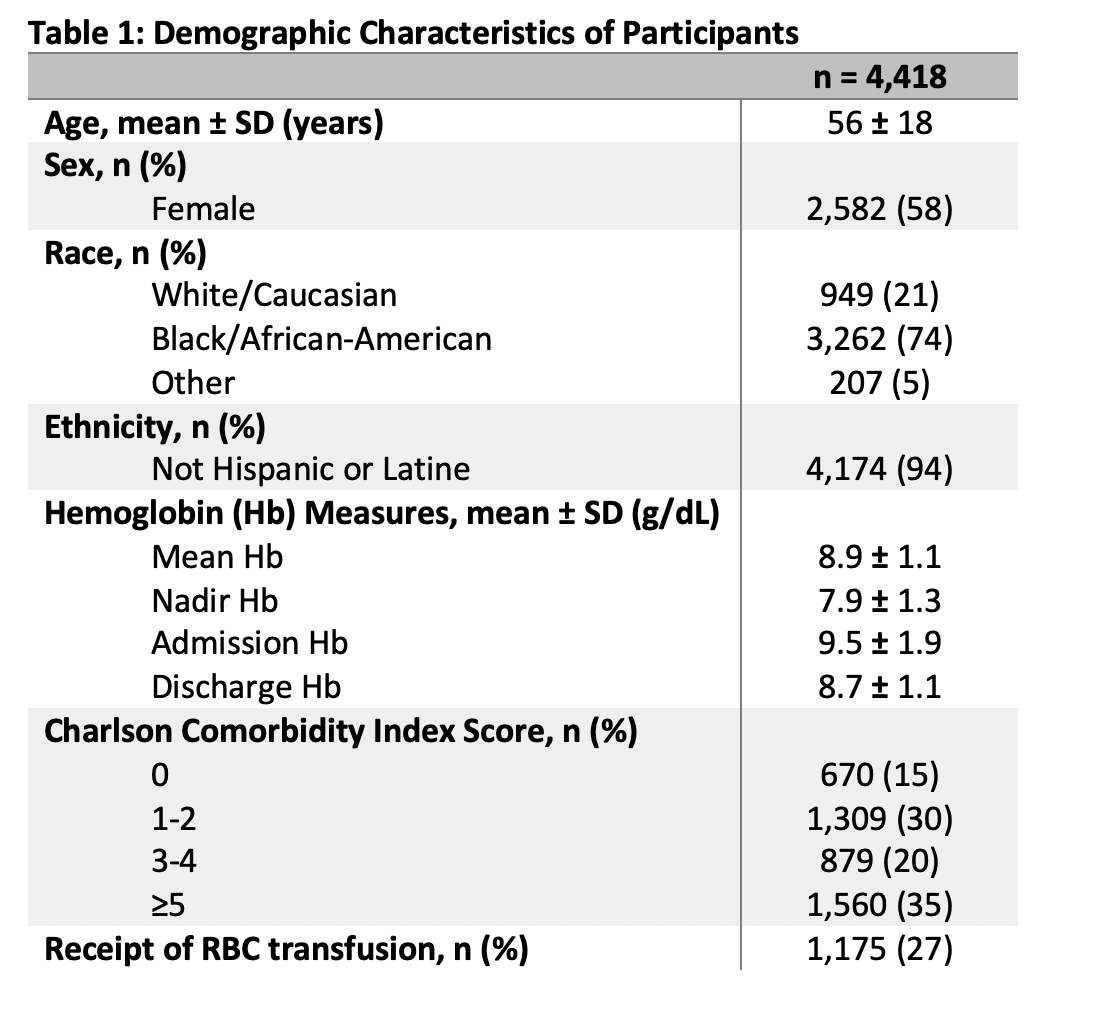
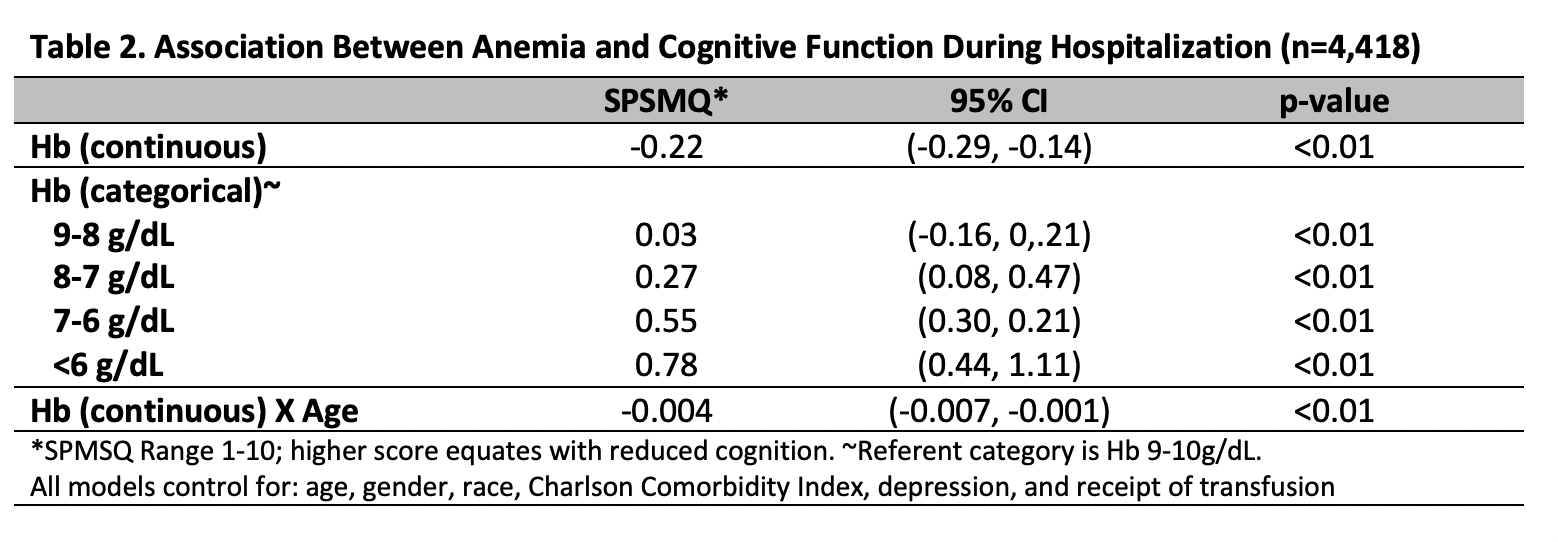
Methods: Hospitalized general medicine patients at an urban academic medical center with a Hb < 10g/dL were approached for an interview at hospital admission. Cognitive function was measured using the Short Portable Mental Status Questionnaire (SPMSQ), which has a range from 0-10 with higher scores indicating worse cognitive function. Patients’ Hb values and clinical data were abstracted from hospital administrative databases. Patients with a diagnosis of dementia were excluded from the analysis. Linear regression was used to test the association between cognitive function (SPMSQ) as the dependent variable and patients’ nadir Hb and age as the predictor variables of interest, controlling for race, gender, Charlson Comorbidity Index, a diagnosis of depression, and receipt of transfusion. An interaction between patient’s nadir Hb and age was also included to test for changes.
Results: A total of 4,418 patients had a Hb< 10g/dL and completed the SPMSQ questionnaire. The average age was 56, 58% were female, and 74% were African American. In the regression models, lower nadir Hb levels were associated with reduced cognition (higher SPMSQ) (β=-0.22, p< 0.01) overall. Additionally, the effect of lower Hb level on reduced cognition was greater within each decreasing Hb strata compared to patients whose Hb was between 9-10g/dL during their hospitalization (Hb: 8-9g/dL, β=0.03, p< 0.01; Hb: 7-8g/dL, β=0.27, p< 0.01; Hb: 6-7g/dL, β=0.55, p< 0.01; Hb< 6g/dL, β=0.78, p< 0.01). The interaction between a patient’s nadir Hb and their age was also associated with significant reductions in cognitive function (β=-0.004, p< 0.01).
Conclusions: Lower Hb levels during hospitalization, particularly the Hb levels tolerated as a result of restrictive transfusion policies, are associated with significant decreases in cognitive function. Clinicians should be aware of and attentive to the effect of anemia on cognitive function, and should consider screening for and monitoring high risk patients with anemia for decreased cognitive function.