Background: When patients are transferred between hospitals (interhospital transfer, IHT), incomplete information exchange between electronic health records (EHRs) poses a barrier to continuity of care. As a result, diagnostic tests may be repeated after transfer, exposing patients to additional risk and adding to costs of care. Shared clinical data between EHRs presents a possible solution. We evaluated the frequency of duplicate diagnostic imaging after IHT from a single community hospital to our tertiary medical center in the year before and after implementation of a shared EHR.
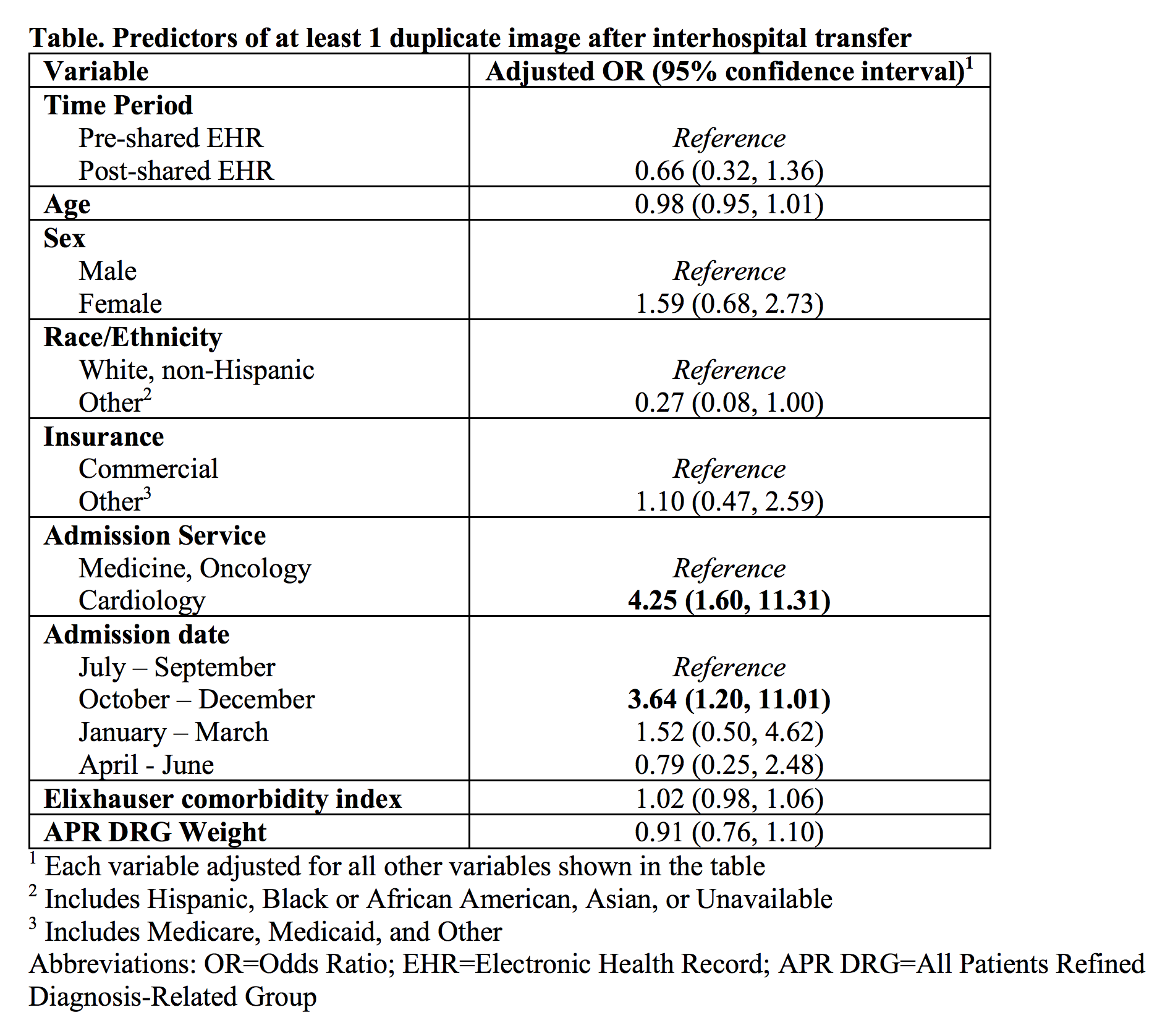
Methods: We identified all inpatients transferred from the community hospital to our general medicine, oncology, or cardiology services in the 1 year before (July 2016-June 2017) and 1 year after (July 2017-June 2018) implementation of a shared EHR. We used administrative data to identify all computed tomography, magnetic resonance image, and ultrasound imaging ordered within the first 48 hours of arrival to BWH, then conducted directed chart review to determine if a duplicate imaging study (defined as same imaging modality and body area) was performed within 7 days prior to transfer. We performed logistic regression to obtain the adjusted odds of transfer with at least 1 duplicate image post- versus pre-shared EHR, adjusting for admission service, time of year, patient demographics, and illness severity (Elixhauser comorbidity score, DRG weight). Secondary analyses examined predictors of transfer with duplicate images across both time periods.
Results: We identified 109 and 92 patient transfers pre- and post-shared EHR, respectively. Patient characteristics were similar between the two groups. Among all 201 transferred patients, 209 imaging studies were ordered within 48 hours after transfer, of which 59 (28.2%) were duplicates. Primary analyses demonstrated a non-significant trend towards decreased transfers with at least 1 duplicate image post- versus pre-shared EHR (20.6% vs. 29.4%, adjusted OR 0.66, 95% CI 0.32,1.36). Secondary analyses demonstrated that transfer to the cardiology service was associated with significantly greater odds of duplicate imaging (OR 4.25, 95% CI 1.60,11.31); there were also seasonal effects (Table).
Conclusions: We found a high frequency of duplicate imaging during IHT, particularly among cardiology transfers. The trend towards decreased duplicate imaging after implementation of a shared EHR suggests that improved health information exchange may be one method to mitigate unnecessary resource utilization during IHT. Further studies with larger sample size should examine whether shared clinical data between EHRs leads to decreased health care utilization during IHTs and evaluate other strategies to reduce unnecessary duplicate diagnostic studies.