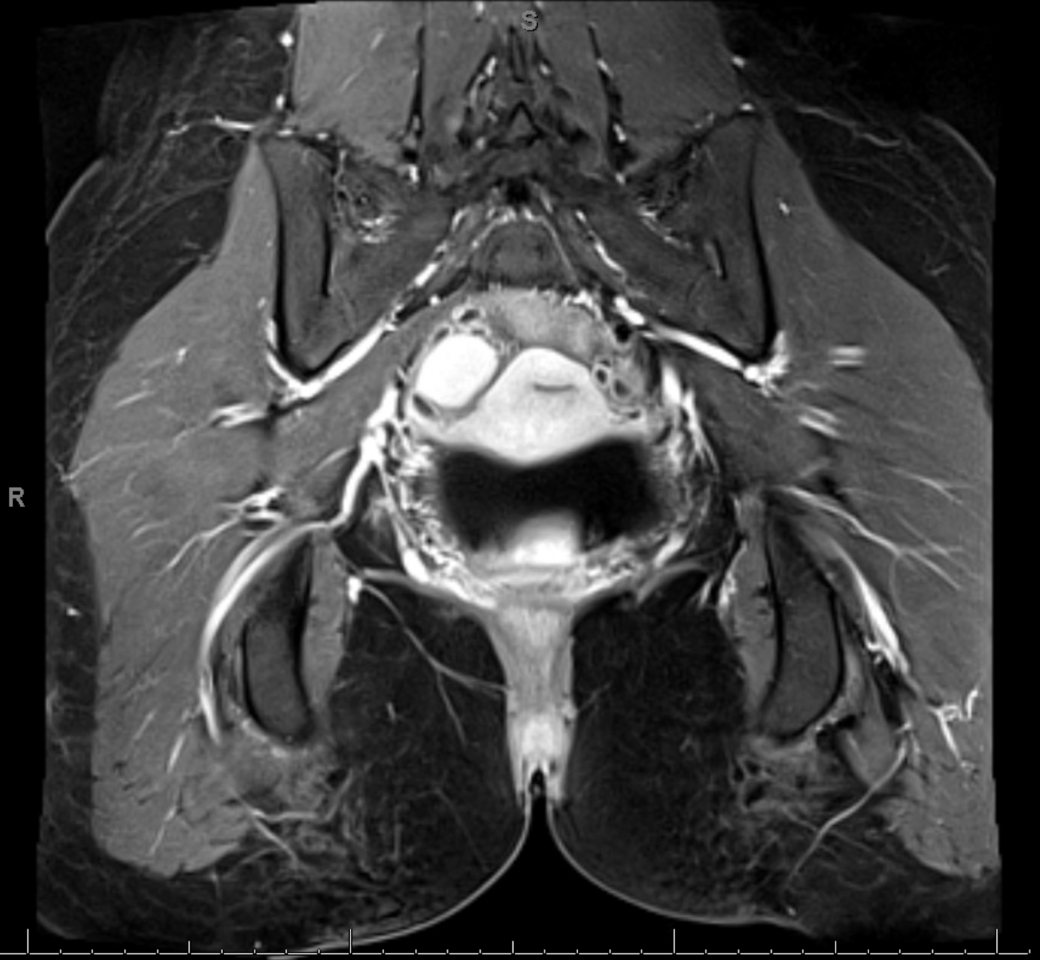
Case Presentation: A 22-year-old female presented with diffuse abdominal pain and a past medical history of endometriosis managed with medroxyprogesterone acetate injections. She also reported a decreased appetite and hematuria. Six months earlier she presented with similar symptoms and was diagnosed with an endometriosis flare. On this admission, the heart rate was 131 bpm, with a systolic blood pressure of 100 mmHg. The exam demonstrated a firm abdomen with diffuse tenderness without peritoneal signs. The basic metabolic panel was notable for a Na of 118 mEq/L, while liver function tests and lipase were normal. A urinary porphobilinogen level was pending. MRI of the abdomen and pelvis showed evidence of extensive endometriosis. She was empirically treated for an endometriosis flare with analgesic medication. However, the pain was refractory to parenteral opioids and required lidocaine and ketamine drips. Urinary porphobilinogen returned elevated alongside a diminished erythrocyte porphobilinogen deaminase activity which resulted in a diagnosis of acute intermittent porphyria (AIP). She clinically improved rapidly with intravenous hemin treatment.
Discussion: The porphyrias are a group of metabolic disorders related to various defects in the biosynthetic pathway responsible for heme production. The most common of these is acute intermittent porphyria (AIP), an autosomal dominant disease caused by mutations in hydroxymethylbilane synthase resulting in deficiency of porphobilinogen deaminase (PBG). AIP typically presents in adulthood with acute attacks precipitated by triggers such as medications (including progesterone), illness, physiologic and psychologic stress, surgery, and fasting (as observed in this patient). Symptoms are thought to arise due to a buildup of cytotoxic precursors, aminolevulinic acid and PBG, which cause direct damage to the peripheral and central nervous systems. Symptoms are nonspecific and variable but often include abdominal pain, tachycardia, hyponatremia, and hypertension. Treatment of AIP involves avoiding precipitating factors and administration of intravenous hemin with a high carbohydrate diet for acute attacks. New preventative treatments are available which utilize siRNA technology.This patient’s diagnosis of endometriosis and previous hospital admission clouded the diagnostic picture and likely contributed to anchoring bias amongst her care providers. Abdominal pain temporally related to hormonal changes can be attributable to AIP, endometriosis, or both concurrently. However, the tachycardia, hematuria, hyponatremia, and pain refractory to parenteral opioids seen in this patient eventually raised suspicion for an alternative etiology.
Conclusions: AIP can present with a myriad of nonspecific symptoms which can lead to underdiagnosis and anchoring bias in the presence of known abdominal pathology. However, abdominal pain refractory to standard analgesic management strategies should raise suspicion and warrant further workup for concurrent pathological processes, such as AIP, until ruled out.