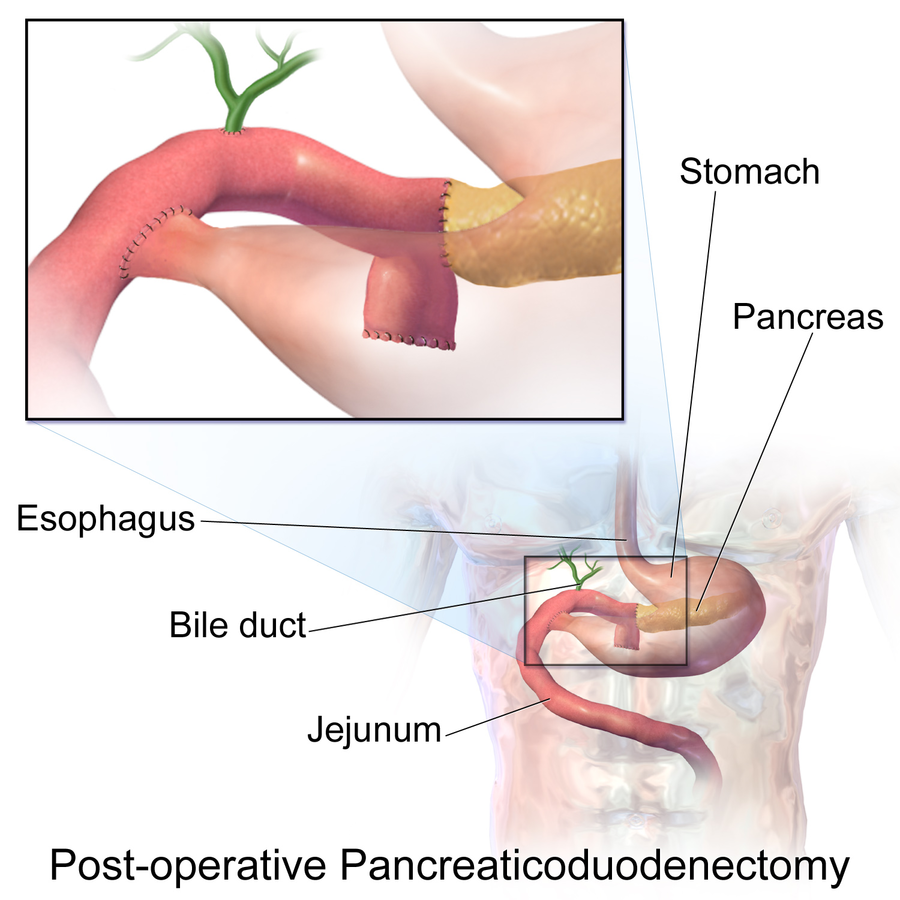
Case Presentation: The presence of abnormal liver function tests has a broad list of differential diagnoses and is commonly seen in patients with medication side-effects. Hepatotoxicity is associated with many checkpoint inhibitor immunotherapeutics and requires immediate initiation of steroids; however, it is important to consider alternate etiologies for transaminitis. We present a case of a patient with presumed medication related hepatotoxicity found to have an extrahepatic etiology to their liver injury.A 69 year-old female with a medical history significant for metastatic pancreatic cancer status-post resection by pancreaticoduodenectomy (Whipple procedure) (Figure 1) presented to the emergency room with complaints of progressive nausea, weakness, malaise, lower extremity edema, dark urine, and abdominal distension. She denied fevers, chills, and abdominal pain. She recently stopped taking pembrolizumab (Keytruda) at the recommendation of her oncologist due to abnormal liver enzymes, but reported progression of her symptoms. In the emergency room, vitals were normal. Physical examination was notable for a chronically ill and frail appearing female with scleral icterus, a distended abdomen, and bilateral lower extremity edema. Laboratory studies were notable for significantly elevated transaminases, but decreased compared to four weeks prior, as well as markedly elevated total and direct bilirubin. She was admitted for evaluation of post-hepatic obstructive pattern. Computed tomography of her abdomen and pelvis with contrast showed increased intra- and extra-hepatic biliary dilation as well as postsurgical changes. The patient underwent endoscopic retrograde cholangiopancreatography with endoscopic ultrasound, and endoscopic biliary decompression was attempted but unsuccessful due to her anatomy. Interventional radiology was consulted for percutaneous transhepatic cholangiography (Figure 2), and the patient successfully underwent biliary cannulation into the small bowel and stent placement. During this procedure, it was noted that there was a stricture of the biliary-enteric anastomosis.
Discussion: This case illustrates the complexity of managing patients with pancreaticobiliary disease. There are many possible complications of the biliary-enteric anastomosis component of pancreaticoduodenectomy (Whipple procedure), including biliary stenosis, bile leak, bleeding, and infections.[1] Biliary strictures are uncommon, with one analysis reporting a 2.6% occurrence rate.[1] The majority of patients who are treated with pembrolizumab have cholestasis prior to medication initiation, and medication related cholestatic injury is common, reported as 14% in one analysis.[2]This case also demonstrates the potential dangers of succumbing to premature diagnostic closure and biases. Confirmation bias causes one to specifically seek information that supports initial conclusions. Other types of bias involve the overvaluation of irrelevant information and persistence of initial beliefs despite new information (anchoring bias). By being open to alternative diagnoses, we were able to recognize the obstructive pattern of liver injury. While infrequent, anatomic causes must remain on the list of differential diagnoses.
Conclusions: In patients with pancreaticoduodenectomy, anastamotic stricture is a possible post-surgical complication to consider. It is also important to be aware of premature diagnostic closure, as well as confirmation and anchoring biases.