Background: The first Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS1) demonstrated that implementation of a medication reconciliation best practices toolkit decreased unintentional medication discrepancies with potential for harm in five hospitals.
Purpose: For MARQUIS2 we utilized lessons learned from MARQUIS1 to implement the toolkit across 18 diverse medical centers.
Description: MARQUIS2 is a real-world, mentored implementation QI study in which we are collecting clinical and implementation outcomes. The modified toolkit includes: 1. Training materials with standardized cases and role-playing to enhance learning and verify competency in taking a “best possible medication history.”
2. Emphasis on the value of trained pharmacy technicians to obtain and document accurate medication histories early in the hospital admission.
3. Increased emphasis on patient and caregiver engagement with input from a patient-family advisory council.
We used a rigorous application process in selecting 18 of 72 health systems to participate. From prior experience, we chose sites as close to the time of implementation as possible, conducted mentor site visits in the first 6 months, encouraged sites to utilize dedicated, trained history-takers, and directed site leaders to secure institutional buy-in and support throughout the project.
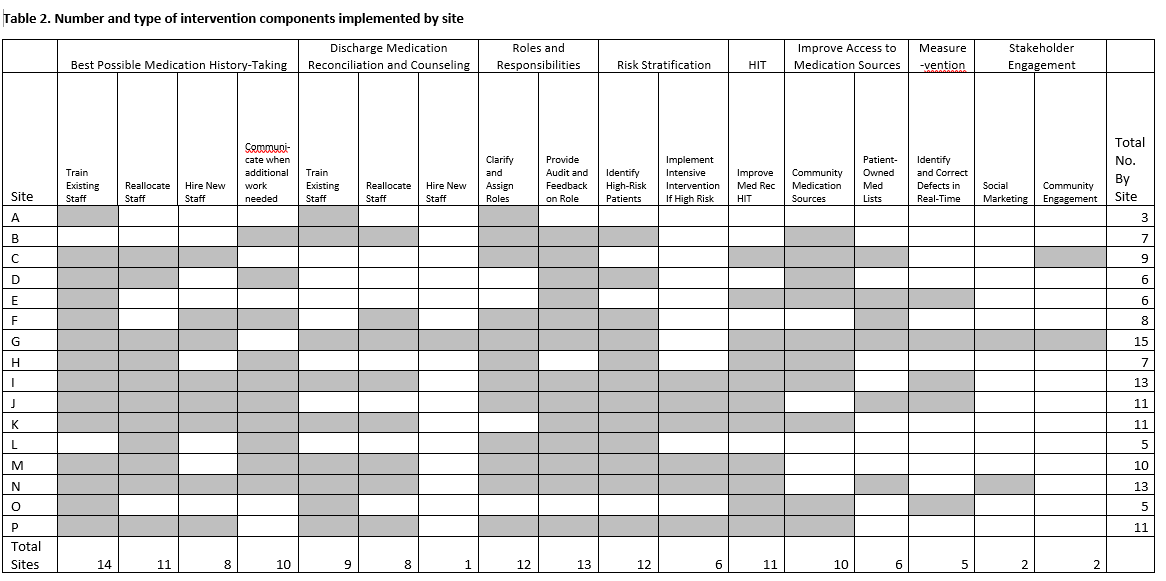
Eight hospitalists mentored the sites via a site visit and monthly phone calls over the 18-month intervention period. With mentor guidance, each site’s local QI team assessed opportunities to improve and implemented one or more of the 17 toolkit components. Sites were provided with an implementation manual, instructional videos, presentations, return-on-investment calculators, quarterly webinars, peer-to-peer learning sessions, an interactive online community, and regional training workshops.
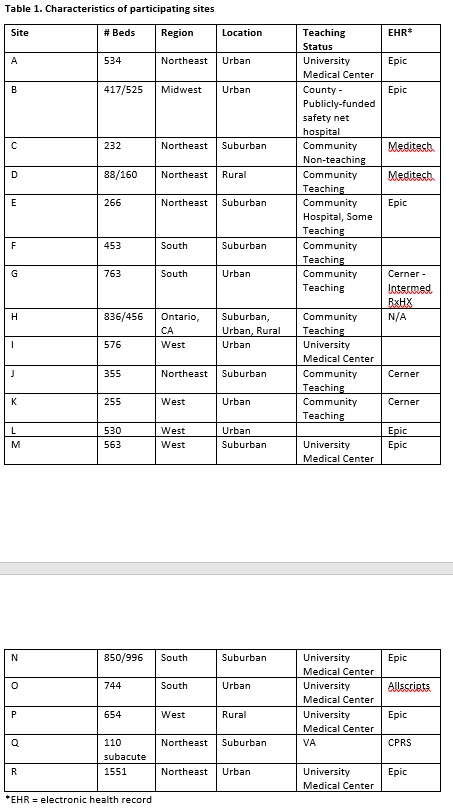
Table 1 displays the 18 participating sites’ characteristics. Sixteen sites have implemented 3 to 15 toolkit components, with 14 sites implementing dedicated BPMH takers and 13 providing audit and feedback on the specific roles and responsibilities among clinical staff (Table 2).
Conclusions: A multi-center medication reconciliation QI initiative using a best practices toolkit and mentors was successfully implemented across 18 medical centers. The most commonly implemented components were incorporating dedicated BPMH takers and defining the roles and responsibilities among clinicians. Different personnel may be needed if sites wish to implement community-based interventions.