Background: Addressing the needs of the geriatric population is critical, as “baby boomers” comprise a larger proportion of hospitalized patients. Hospitalists increasingly care for these complex geriatric patients. The “BEERS Criteria” are evidence-based guidelines that encourage medication safety by describing potentially inappropriate and harmful medications (PIMS) among geriatric patients. BEERS guidelines recommend that with a few exceptions, benzodiazepines should be avoided in older adults as they can increase the risk of cognitive impairment, delirium, and/or falls. Despite these guidelines, little is known about the extent to which hospitalists adhere to these guidelines. This study is aimed to characterize patterns of hospitalist adherence to BEERS guidelines for prescribing and monitoring benzodiazepines for older adults.
Methods: We conducted a retrospective chart review based on electronic health records from a large Midwest hospital. Subjects were admitted patients aged 70-85 years who were seen by a hospitalist over a one-year period (Jan-Dec 2017) and who had been prescribed a benzodiazepine while in the hospital. Two independent reviewers reviewed 351 patient charts where benzodiazepines were prescribed during hospitalization as per inpatient pharmacy records, including admission and progress notes. Key elements noted were the adequacy of documentation and the rationale for prescribing the benzodiazepine. “Adequate” charts were classified as those with proper documentation and a stated rationale for prescribing benzodiazepines in the note’s impression and plan. “Partial” documentation was defined as the inclusion of rationale and the prescription of benzodiazepines in the note but missing from the impression and plan. “Missing” was defined as no documentation or rationale found for prescribed benzodiazepines. Data was entered into REDCap, and analyzed with R. Student’s t-test and chi-square tests to determine any association between the care team information, patient data, and if the prescription followed the guidelines (p-value of <0.05 was statistically significant).
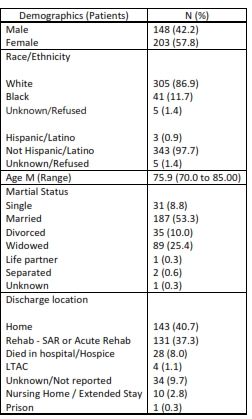
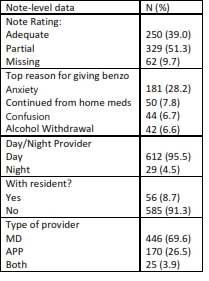
Results: Charts from 351 patients were analyzed, which included 641 separate notes. The patient sample was 57.8% female, and the mean age was 75.9 years. 40.7% were discharged home and 37.3% were discharged to rehab (see table 1). Based on the rationale provided in the notes, 28.2% of benzodiazepines were prescribed to address anxiety, which is inconsistent with the BEERS criteria. Based on the quality of progress note documentation for the 641 notes, 39% were adequate, 51.3% were partial and 9.7% had missing data. 95.5% of the documentation were provided by the day-team providers, which included MDs, APPs or both; 8.7% of encounters included residents (see table 2). Based on the p-value (<0.05), adequate and partial documentation did not follow guidelines and physicians tended to follow the guidelines more than advance practice providers. In their assessment of each note, reviewers found evidence of “copy and paste” techniques where verbatim information was re-used from previous encounters. For those notes, no clear determination could be made about guideline adherence.
Conclusions: Hospitalists in this medical center inappropriately prescribe benzodiazepines in older patients. This suggests a persistent need for continuous education for hospitalist on current guidelines on prescribing benzodiazepines to the geriatric population.