Background: Elevated blood pressure (BP) is common among hospitalized patients, with prevalence estimates between 50-70%. Many factors may contribute to this, such as pain, nausea, anxiety, or volume overload. However, true hypertensive emergency requiring rapid reduction in BP is relatively rare. The easy availability of intravenous (IV) antihypertensives may lead to unnecessary treatment of asymptomatic patients and resultant adverse medication effects. The objective of this study was to describe the prevalence and effects of using IV antihypertensive medications in asymptomatic inpatients on a general medicine service, and to assess the need for a targeted initiative to reduce overutilization.
Methods: We obtained computerized electronic health record (EHR) data from patients hospitalized on the acute care general medicine service at an 800 bed tertiary-care hospital between 1/2017 and 10/2017 and identified all patients who had at least 1 documented episode of elevated blood pressure (>140/90 mmHg). Patients were categorized as “asymptomatic” if they had no diagnostic tests for end-organ damage (i.e. electrocardiogram, serum troponin, chest x-ray, computerized tomography scan of the head) in the 1 hour preceding, or 15 minutes following, administration of an IV antihypertensive medication, and were without a primary diagnosis code of a condition where aggressive treatment of hypertension is medically indicated (e.g. myocardial infarction, stroke, intracranial hemorrhage). The date and time of all IV hydralazine and labetalol administrations were obtained from pharmacy records, along with pre- and post-treatment vital signs.
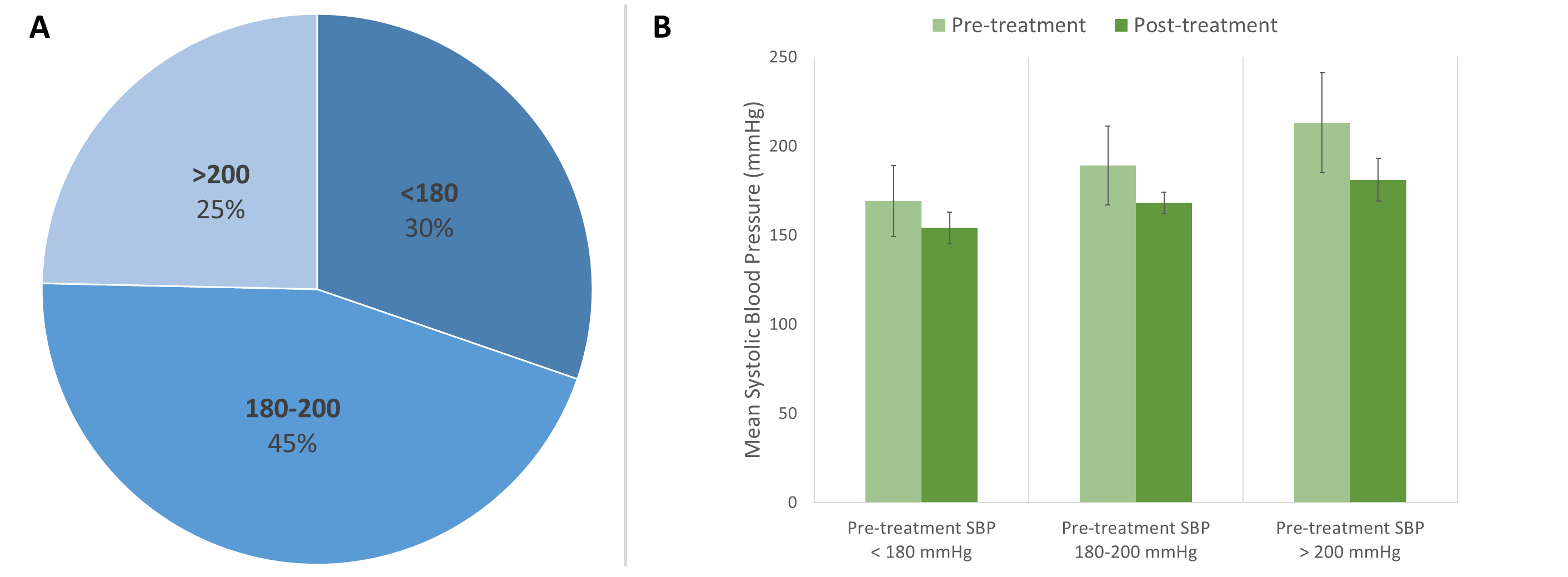
Results: We identified 3,774 patients with greater than or equal to 1 episodes of asymptomatic elevated BP. Of these, 279 (7.4%) received IV hydralazine and/or labetalol during their hospitalization. On average, patients received 2.4 doses of IV antihypertensives (range: 1-30); 60% of doses administered were hydralazine. The majority (426 [63%]) were ordered on a standing “prn” basis, while 248 (37%) were ordered as a one-time dose. Mean pre-treatment BP was 189/90 ± 18/19 mmHg; 30% of pre-treatment systolic blood pressures (SBP) were < 180, and 75% were < 200 mmHg (see figure 1). BP fell on average by 22/9 mmHg, with mean post-treatment BP of 167/81 ± 25/18 mmHg; however, 17% had either no change, or an increase in BP, following treatment. Eighty-seven patients (14%) had a decrement in SBP >25%.
Conclusions: We found that ~ 1 in 13 medical inpatients received IV antihypertensives for asymptomatic elevated BPs, that treatment was often initiated for only modestly elevated BP, and that clinical response was highly variable. Although our study cannot describe associations with clinical outcomes, this likely represents a valuable opportunity for efforts to reduce unnecessary treatment and avoid patient harm.