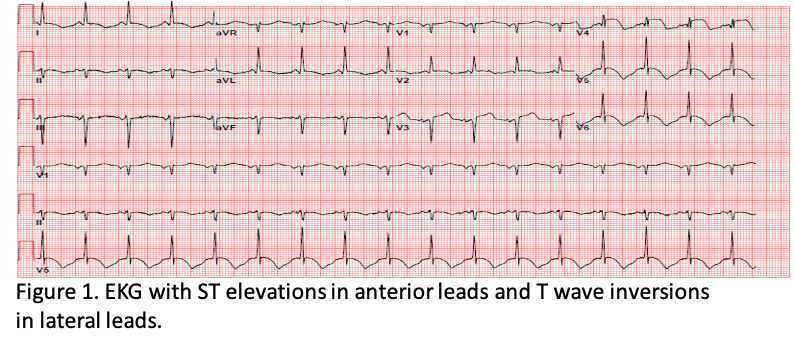
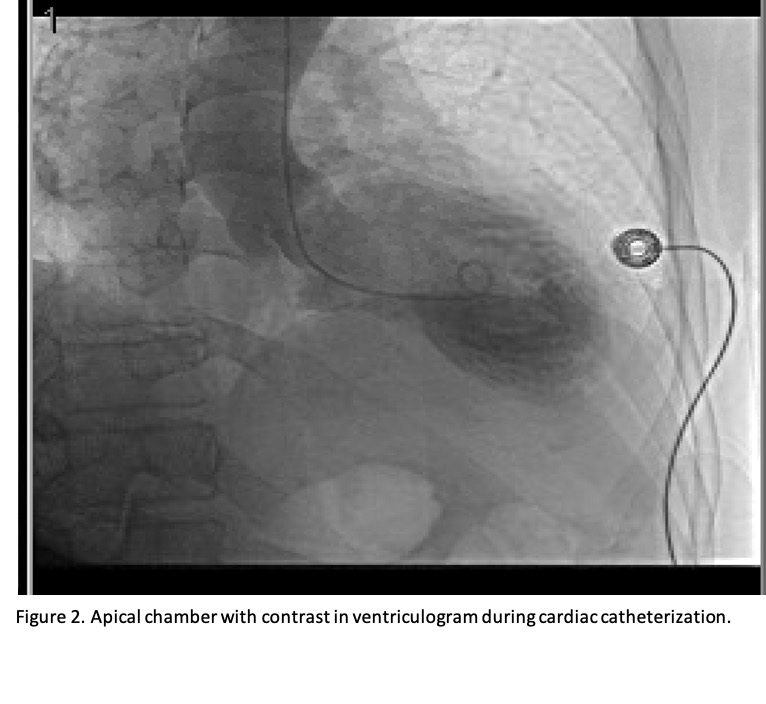
Case Presentation: A 67 year-old male presented to the hospital with progressive weakness, lightheadedness upon standing, and intermittent chest pain. His medical history includes hypertension and chronic back pain from spinal stenosis for which he was previously on long-term prednisone. Two months prior to admission he underwent an uncomplicated lumbar fusion with discectomy after which his symptoms began and worsened leading to this hospitalization. His inpatient workup was significant for profound orthostatic hypotension. An EKG showed new ST elevations in anterior leads (Fig. 1). A STEMI alert was called and an urgent cardiac catheterization revealed moderate non-obstructive coronaries and apical ballooning on ventriculogram consistent with Takotsubo Cardiomyopathy (Fig. 2). Troponin I peaked at 0.38ng/ml, and an echocardiogram confirmed a newly reduced ejection fraction of 30%. Of note, prior to surgery, he had a cardiac catheterization showing non-obstructive coronaries and an echocardiogram with normal wall motion and ejection fraction. His post-op EKG and troponin were also at baseline. Upon further review, the patient reported abrupt cessation of his prednisone after spinal surgery to promote healing. He was previously taking 20mg daily for many years, and was not given instructions to resume or taper his steroids after surgery. An inpatient morning cortisol level was low at 3.8 ug/dL and one-hour 250mcg cosyntropin stimulation test was inadequate at 5.4 ug/dL, consistent with adrenal insufficiency due to exogenous steroid use. Endocrinology was consulted and he was started on stress-dose steroids with marked improvement in symptoms. He was tapered to a physiologic dose on discharge. It was thought that his cardiomyopathy was associated with adrenal insufficiency.
Discussion: Adrenal insufficiency is a common occurrence in patients who have prolonged exogeneous steroid use[1]. A meta-analysis found that even those using intranasal, topical, or intra-articular forms of steroids are at high risk of developing secondary adrenal insufficiency [1-4]. A few case reports have linked Takotsubo Cardiomyopathy to adrenal insufficiency in adults [2]. The exact cause of stress cardiomyopathy is unknown, but catecholamines are believed to play a major role. Glucocorticoids are thought to be important in maintaining intracellular calcium concentration and membrane calcium transport function in cardiomyocytes, thereby regulating cardiac contractility [5]. In addition, glucocorticoids are believed to promote microsomal phosphorylase activity in the myocardium, the reduction of which may impair glycogenolysis and cardiac excitation-contraction coupling [2, 6]. Taken together, adrenal insufficiency may lead to impaired cardiac function and potentially stress cardiomyopathy.
Conclusions: Glucocorticoids are thought to play a major role in maintaining cardiac contractility and function. As such, adrenal insufficiency may lead to stress cardiomyopathy. Given the frequency of both conditions, it is important to recognize this reversible cause of stress cardiomyopathy as it relates to adrenal insufficiency. In addition, peri-operative steroid use should be monitored closely to avoid complications associated with abrupt cession of chronic steroids.