Background: Late discharges are associated with hospital overcrowding, delayed inter-unit patient transfers, lower patient satisfaction scores and longer length of stay. At our hospital, there has been a consistent discordance between the teaching and non-teaching hospitalist services in the percentages of patients discharged before 11 am, which was 8.4% (teaching teams) versus 36.4% (non-teaching teams) within a one-year period. Historically, much of the emphasis is placed on faculty members to promote early patient discharge. Resident trainees are frontline providers and are well suited to identify and conduct early discharges. We aim to implement a resident driven multi-step intervention to improve discharge rates before 11 am on the general medicine teaching teams. Our objectives were: (1) To design and implement a quality improvement initiative to increase discharge rates before 11am on inpatient general medicine teaching teams; and (2) To evaluate the effectiveness of this initiative in terms of early discharge rates, length of stay (LOS), 30-day readmission rates and resident perception.
Methods: We used the PDSA model of quality improvement to test a multistep intervention on all inpatient general medicine teaching hospitalist teams at a tertiary care academic medical center. The study was initiated on August 2017 and is presently ongoing. Prior to the study, we conducted retrospective chart review of 1556 patient encounters to obtain baseline data on discharge orders placed before 11am. From June 2015 to June 2016, the early discharge rate for teaching teams was 8.4% in comparison to 36.4% on the non-teaching teams. In the first PDSA cycle of the study, all general medicine residents underwent an early discharge didactic and received a checklist tool with instructions on how to conduct daily discharge walk rounds with their attending physicians on patients eligible for discharge the next day. Early discharge resident champions were identified to serve as leaders and sent electronic pages and in-person reminders to have discharge orders in before 11am. In PDSA cycle two of the study, geographical distributions of patients were created to enable formal multidisciplinary discharge huddle. We measured overall early discharge rate before 11am (DC-11), length of stay (O/E ratio), 30-day readmission rates after each PDSA cycle. Additionally, we measured overall resident perception five months after the intervention.
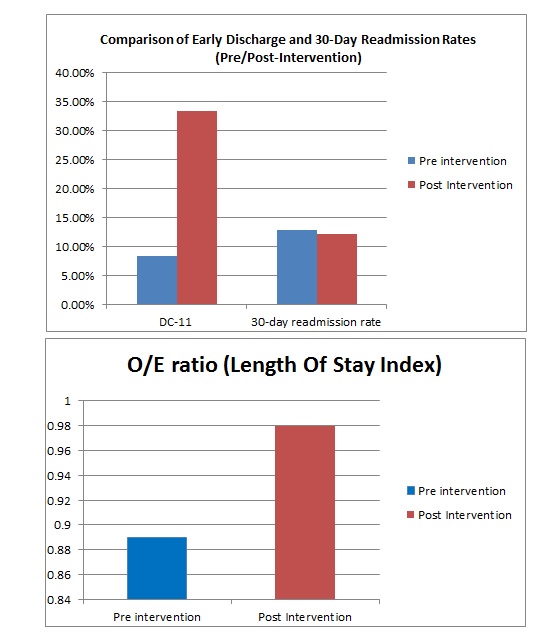
Results: Two months after the initiation of PDSA cycle one (discharge walk rounds and didactic), DC-11 rates increased from 8.4% to 24.8%. After PDSA cycle 2 (DC huddle and geographic units), DC-11 rates increased to 42%. O/E length of stay index went from 0.89 pre-intervention to 0.98 post-intervention, and 30-day readmission rates remained the same at 12.93% pre intervention/12.2% post intervention. Overall 55% of the residents ‘agreed’ or strongly agreed’ that the discharge initiative enabled them to understand prioritization of early patient discharge. In addition, 45% of the residents ‘disagreed’ or ‘strongly disagreed’ that early discharge compromised their learning on teaching rounds.
Conclusions: Our study demonstrates that a resident driven approach that entails educational didactics, checklist tool, resident walk rounds and multidisciplinary discharge huddle can successfully lead to significant improvements in early discharge rates. Thus, DC-11 is an achievable goal, not only for non-teaching teams but also for resident-run teaching services.