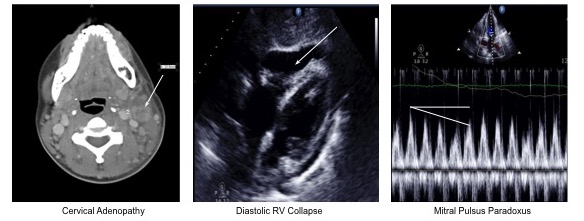
Case Presentation: A 29-year-old African-American female presented with two weeks of left neck swelling and fever. Over four months, she had noted fatigue, cough, night sweats, and an unintentional 12-pound weight loss. Two empiric courses of antibiotics effected no clinical change. She had no toxic habits and was sexually active with one male partner. Travel history was notable for visits to Haiti and Colombia. Triage vitals were notable for fever and tachycardia. Exam disclosed tender bilateral cervical adenopathy most prominent on the left, with overlying soft tissue swelling. Labs were notable for pancytopenia and a mildly elevated lactate dehydrogenase. Computed tomography (CT) revealed bilateral pleural effusions, splenomegaly, abdominopelvic ascites and adenopathy. CT neck revealed adenopathy of the left cervical chain with surrounding soft tissue edema. Evidence of central necrosis or suppuration in the largest node was thought to be most compatible with infection or malignancy. Otolaryngology, infectious disease, and hematology services were consulted. Empiric antibiotics started on admission were discontinued after an extensive, non-diagnostic infectious evaluation. Although flow cytometry of peripheral blood and bone marrow were normal, an excisional node biopsy revealed reactive follicular hyperplasia with polyclonal plasmacytosis, findings suggestive of angioimmunoblastic T-cell lymphoma. She was discharged in stable condition with plan for outpatient workup of presumptive lymphoma. Two days later she returned to the hospital with acute chest pain and dyspnea. She was found to have cardiac tamponade, requiring emergent pericardiocentesis. She was admitted to the intensive care unit where rheumatologic workup revealed positive anti-nuclear antibody and positive anti-Smith antibody, establishing a diagnosis of systemic lupus erythematosus (SLE). She responded favorably to standard therapy and was discharged in stable condition.
Discussion: Although the presentation of SLE is classically associated with fever, arthritis, and malar rash, adenopathy can sometimes dominate the clinical picture, causing the disease to mimic infection or hematologic malignancy. Indeed, one case series estimates the prevalence of adenopathy during the active phase of illness to lie between 12% and 59%, most commonly cervical (46%) and axillary (43%). In this case, the presence of adenopathy and plasmacytosis, present in 17% of SLE patients with peripheral cytopenias, guided thinking toward lymphoma, thereby delaying a correct diagnosis.
Conclusions: Although more typical of infection or neoplasm, adenopathy and plasmacytosis may dominate the presentation of SLE, so their presence should always prompt a rheumatologic workup.