Background: It is imperative for Physician Assistant (PA) students to be exposed to hospital medicine as 40% of practicing PAs identify the hospital as their principal clinical practice setting (1). Many of these rotations were cancelled due to the COVID-19 Pandemic, negatively impacting the 70% of PA programs not affiliated with an academic medical center (2). To address this need and provide a comparable experience for PA students, medical educators at University of Chicago created a Virtual PA Rotation (VPAR).
Purpose: Develop a high-yield clinical rotation for private PA programs negatively impacted by COVID-19 by implementing and evaluating a four-week long VPAR comprised of 1) direct patient care, 2) medical educator facilitated breakout sessions, 3) asynchronous learning.
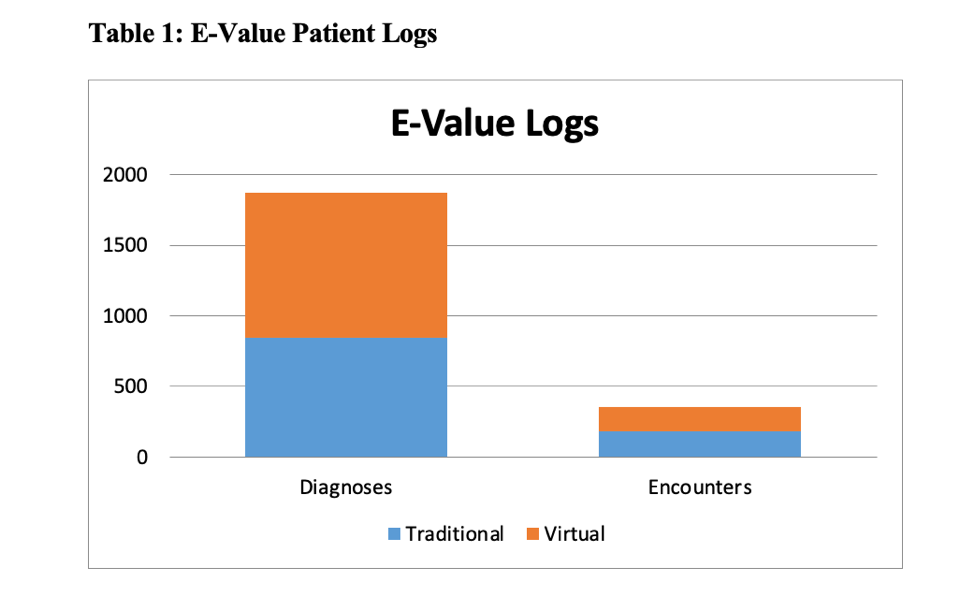
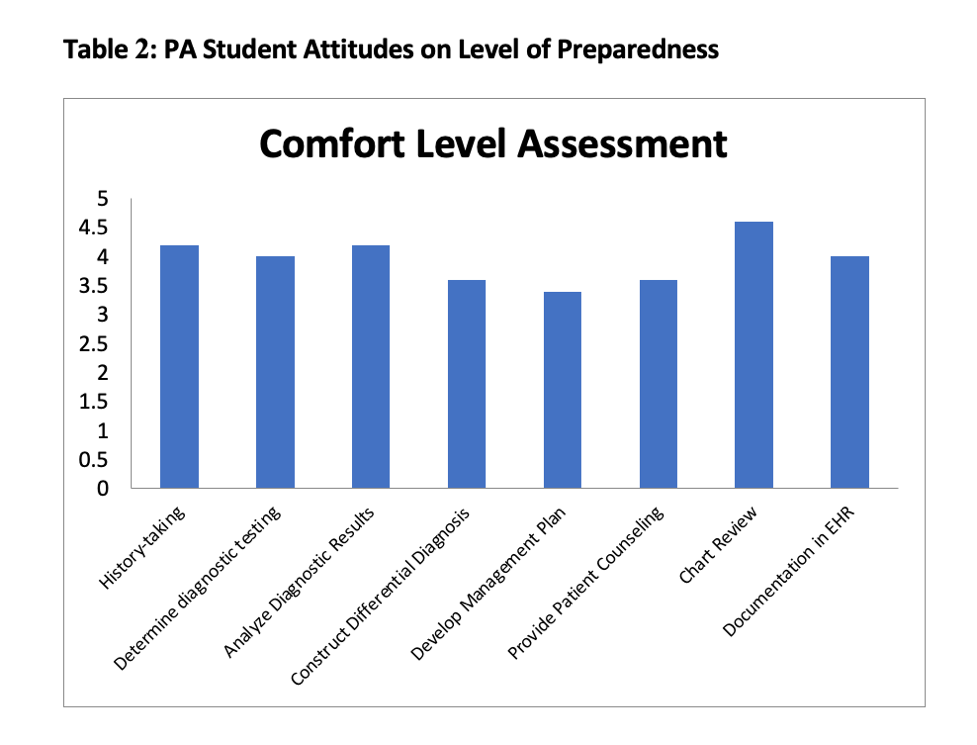
Description: Five students worked with three preceptors for the VPAR and were assigned 3-6 patients daily. Direct patient experiences included virtual interviews, preceptor staffing and completion of daily progress notes. This was augmented with medical educator-facilitated breakout sessions and asynchronous didactic sessions via Zoom. Evaluation of the VPAR included: 1) comparison of virtual vs traditional in-person rotation patient logs, 2) post-curriculum survey of students and medical educators satisfaction and self-efficacy, 3) student pass rate on end of rotation (EOR) examination. Students recorded seeing 171 patients virtually with 1030 diagnoses, similar to the 182 patients and 845 diagnoses from 2019 in-person rotations (Table 1). 5/5 students completed the post-survey. Educational activities that closely mimicked in-person rotations, such as interviewing patients, case presentations and discussions with preceptors, were rated as most useful on a 5-point Likert-scale. Students felt most prepared in their ability to review charts, analyze results and obtain a patient history (Table 2). 5/5 students felt this was an adequate experience to understand hospital medicine. 100% of students passed their EOR exam. 59% (13/22) of medical educators completed the post-survey. 85% (11/13) were moderately or extremely satisfied with the VPAR, 77% were moderately or extremely likely to recommend the VPAR to other educators, and 100% felt this experience made them more open to interprofessional teaching. Lessons learned from the main preceptors included limitations of technology such as decreased device battery life, need for troubleshooting and loss of organic educational experiences for students. They also highlighted concerns regarding increased time dedicated to logistics of the rotation while managing highly complex patients.
Conclusions: We were able to create an innovative, high-yield internal medicine hospital rotation to meet the need for PA students negatively impacted by COVID-19. The VPAR overall was a success as measured by 100% EOR examination pass rate, high student ratings, and comparable patient encounters and diagnoses. The VPAR was also well-received by medical educators, though most felt it was more time-consuming, proving to be the biggest limitation to this model. However, as COVID-19 continues and health systems respond, a VPAR is a reasonable alternative to in-person clinical rotations. Additionally, this pilot rotation’s success demonstrates that VPARs may be an interesting addition to PA education, particularly for unaffiliated programs with a significant need for access to inpatient rotations and tertiary care centers.