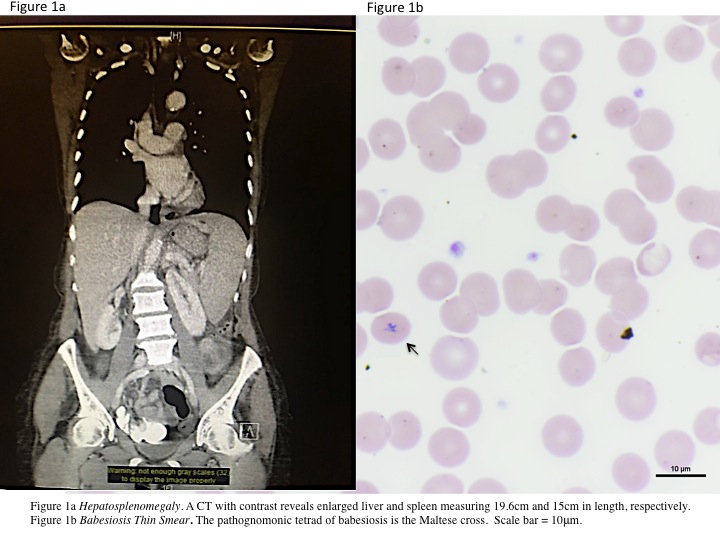
Case Presentation: A 71 year old woman with a history only significant for Lyme disease in 2005 presented with complaints of malaise and fatigue for two weeks. One week prior to admission, the patient was evaluated by her physician who prescribed a course of doxycycline, after recognizing the patient was bitten by a tick in the Catskills three months earlier. At a one-week follow-up visit, she was advised to go to the emergency room for increasing fatigue, developing jaundice, and worsening shortness of breath. The patient reported subjective fevers and orange-colored urine over the course of her two-week illness. She denied rashes or sick contacts. She drinks alcohol occasionally and has no reported tobacco use. In the Emergency Department, the patient was afebrile with stable vitals. Her examination was significant for jaundice, scleral icterus, and positive jugular venous pulsations to the ear at 90 degrees. Her abdomen was tender in the right upper quadrant, with prominent hepatosplenomegaly. Labs were notable for anemia (hemoglobin 6.5), reticulocytosis (3.7%), thrombocytopenia (48,000), haptoglobin <7, bandemia (17%;WBC 5.0), hyponatremia (126), direct hyperbilirubinemia (total 12.2, direct 9.2), elevated transaminases (AST/ALT 45/148), high alkaline phosphatase (182), elevated LDH (1062), and urine urobilinogen of 4.0. A CT with contrast showed an enlarged liver (19.6 cm) and spleen (15 cm) (Figure 1a). Microbiology thin smear results established Babesia microti parasitemia at 5% (Figure 1b), confirmed by PCR, after which the patient was treated with quinine and clindamycin. Her hospital course was complicated by bilateral cinchonism and acute respiratory distress syndrome, thought secondary to possible quinine toxicity and advanced babesiosis, respectively. She was transitioned to a seven day course of atovaquone and azithromycin and transferred to the MICU for increasing O2 requirements. There, the patient later recovered, lab values normalized, and blood analysis for parasitemia was undetectable after four days of treatment.
Discussion: Numerous individual case reports describing clinical outcomes associated with babesiosis aim to highlight epidemiological trends of this rare and debilitating tick-borne illness. Though the disease ranges in severity, often history and laboratory values steer the clinician toward the diagnosis. Classically, infection with Babesia microti causes a hemolytic anemia and resulting indirect hyperbilirubinemia. However, our patient’s presentation of profound direct hyperbilirubinemia, which resolved after initiation of antibabesial therapy, is unique. To date, only two case reports describe direct hyperbilirubinemia in adult babesiosis though levels are more modest (3.1; 4.2). Though the pathogenesis of direct hyperbilirubinemia in babesiosis is unclear, we suspect that in our patient it is of hepatobiliary origin, consistent with her striking hepatosplenomegaly. Furthermore, our patient’s extensive hemolysis may contribute to biliary sludging.
Conclusions: Hemolytic processes including tick-borne illnesses, when severe, have the potential to elevate both indirect and direct bilirubin. This case underscores the importance of carefully evaluating peripheral blood smears in any patient who presents with indirect or direct hyperbilirubinemia and suspected history of a tick bite.