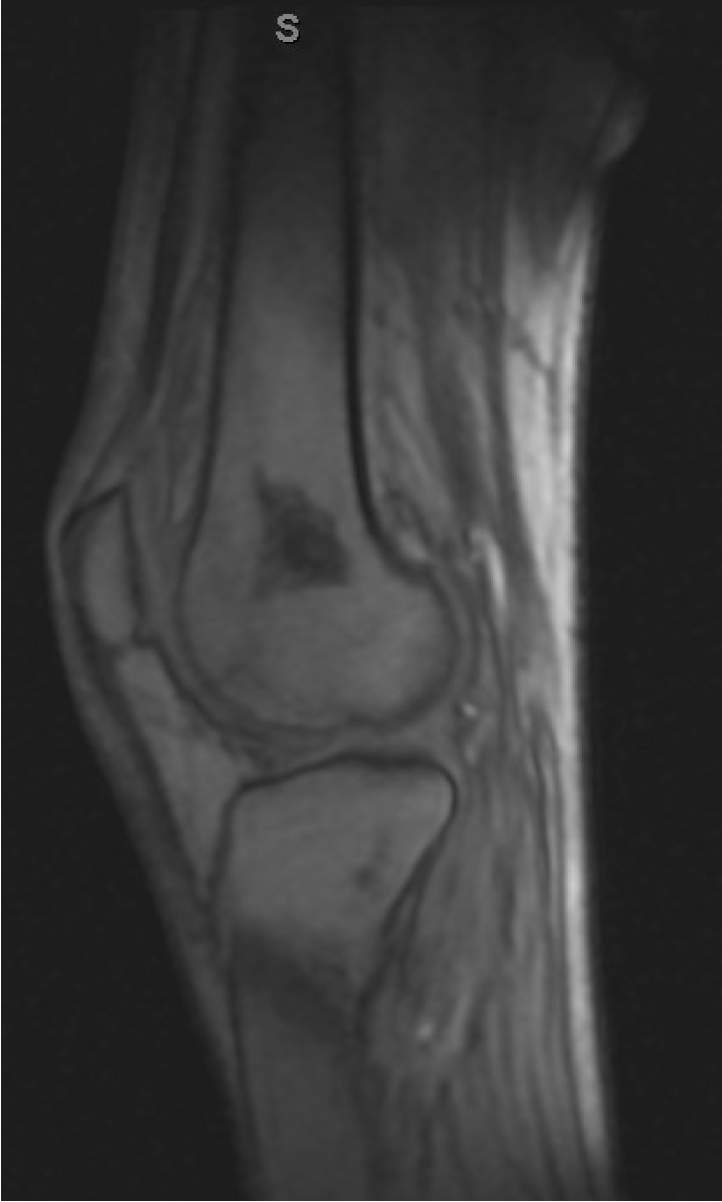
Case Presentation: A 48-year-old man with end-stage renal disease due to IgA nephropathy underwent a deceased donor kidney transplant in 2008, which resulted in graft failure. A second transplant in 2019 required additional thymoglobulin due to high panel reactive antibodies and was complicated by BK nephritis, treated with leflunomide. Since treatment, he had persistent leukopenia, absolute lymphocytopenia and had been on chronic immunosuppressive therapy with mycophenolate, tacrolimus and prednisone. He presented with an eight-month history of oropharyngeal pain, odynophagia, significant 30-pound weight loss, and progressive right ankle pain. Examination revealed white plaques and two shallow ulcers with erythematous borders on the tongue; his ankle had marked swelling and tenderness. Initial treatment for suspected oropharyngeal and esophageal candidiasis failed. Tests for HIV , CMV , EBV , and BKV, were negative. Laryngoscopy showed asymmetric tongue base fullness; EGD was unremarkable. A biopsy of the tongue lesion eventually revealed intracellular fungal elements consistent with Histoplasma capsulatum, prompting a positive quantitative urine Histoplasma antigen (1.6 ng/mL). Patient was then admitted for further treatment and imaging. A CT scan showed a calcified granuloma in the right lung and bilateral adrenal nodules measuring 15 and 11mm, while an MRI revealed ankle and knee tenosynovitis. The lung granuloma was presumed to be the site of latent infection, with additional findings indicative of disseminated disease. Treatment included prednisone for physiological adrenal replacement, posaconazole, and discontinuation of mycophenolate, leading to significant improvement. However, new left knee tenosynovitis developed ten days into treatment. The patient’s urine antigen levels decreased by 50%, and he was discharged with a plan to complete 12 months of antifungal therapy, depending on clinical evolution and follow-up.
Discussion: Histoplasmosis, caused by Histoplasma capsulatum, often presents with mild respiratory symptoms or asymptomatically in immunocompetent individuals. In contrast, disseminated histoplasmosis is a severe condition in immunocompromised patients, where the disease frequently exhibits atypical and nonspecific symptoms, complicating diagnosis.This case highlights the uncommon presentations observed on immunocompromised patients. Oral ulcers and tenosynovitis are very rare manifestations of histoplasmosis but can occur in patients with significant immunosuppression. Tenosynovitis is especially rare, with few documented cases, often in patients on chronic immunosuppressive therapy, potentially linked to immune reconstitution inflammatory syndrome due to the interruption of immunosuppressive therapy.
Conclusions: The atypical presentation in this patient delayed the diagnosis, leading to disease progression before antifungal treatment was initiated. Histopathological and radiologic diagnosis were critical to identifying the etiology and extent of the disease. This underscores the need for rapid histopathologic diagnosis when facing an atypical case presentation. As well as considering uncommon presentations and conduct thorough diagnostic evaluations, having the awareness that atypical symptoms and rare infections can present in immunocompromised patients such as kidney transplant recipients, to ensure prompt and appropriate intervention.