Case Presentation: Sweet Syndrome, also known as acute febrile neutrophilic dermatosis is an uncommon inflammatory disorder of skin characterized by abrupt eruption of painful, edematous, erythematous papules, plaques, nodules and rarely bullous lesions in addition to involvement of mucous membranes, musculoskeletal system and internal organs. There are very few cases reported with sweet syndrome (mostly non-bullous type) from radioiodine contrast, especially in patients with ANCA vasculitis. We report the first case of bullous variant of sweet syndrome as a complication of IV contrast use.
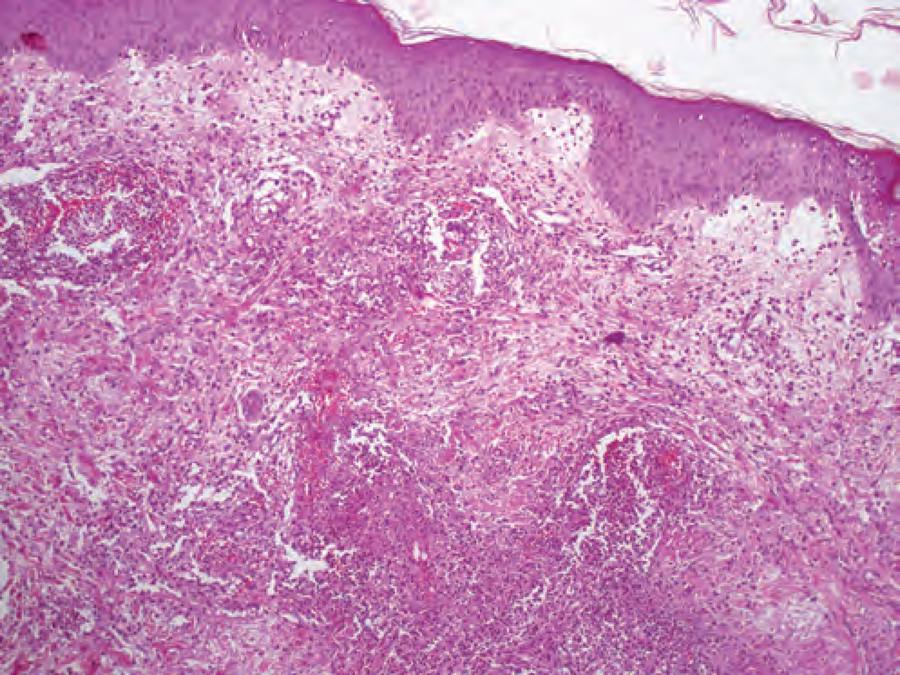
73-year-old male with past medical history of ESRD on hemodialysis secondary to ANCA vasculitis presented with sudden onset of nodular/ bullous hemorrhagic lesions that initially erupted at the back of neck gradually progressed to face, head and upper torso. On admission, patient also complained of photophobia and fatigue. In the past, he reportedly had hives after radioiodine contrast use. A week prior to presentation, he was diagnosed with ascending colitis on CT abdomen w/ contrast, which resolved with ciprofloxacin and metronidazole, confirmed by a repeat CT abdomen w/ contrast before discharge. Work up on the current presentation was significant for leukocytosis of 12000, neutrophilia of 10400, thrombocytopenia, erythrocyte sedimentation rate of 33 and CRP of 18.1. Biopsy of the skin lesion revealed a diffuse infiltrate of neutrophils with prominent edema in the superficial reticular as well as papillary dermis, indicative of acute febrile neutrophilic dermatosis. The skin lesions resolved with 40mg of prednisone.
Discussion: Sweet syndrome can be divided into classical, malignancy-associated and drug-induced sweet syndrome. Our case was a rare bullous variant of sweet syndrome secondary to underlying IV contrast use. Bullous variants have been reported in hematological malignancies, but not in relation to drugs, especially never with IV contrast use (1). Our patient met all the criteria for drug-induced sweet syndrome except fever. Criteria include, abrupt onset of painful erythematous plaques and nodules; histopathological evidence of a dense neutrophilic infiltrate without leukocytoclastic vasculitis; temporal relationship with drug use and clinical presentation with resolution of symptoms after steroid treatment. This disorder mainly affects 30-70 age group and reportedly has a female predominance. Pathogenicity is due to cytokine dysregulation. There are theories about elevated blood G-CSF levels, which are known for prolonging survival rates of neutrophils, eventually resulting in increased oxidative metabolite production, chemotaxis and phagocytosis(2). Elevated G-CSF are also found in ANCA vasculitis, which makes patients more susceptible to developing Sweet syndrome in the presence of triggers like radioiodine contrast.
Reference
1. Voelter-Mahlknecht S1, Bauer J, Metzler G, Fierlbeck G, Rassner G, Int J Dermatol. 2005 Nov;44(11):946-7.
2. Kawakami T, Ohashi S, Kawa Y, Takahama H, Ito M, Soma Y, Mizoguchi M. Elevated serum granulocyte colony-stimulating factor levels in patients with active phase of sweet syndrome and patients with active behcet disease: implication in neutrophil apoptosis dysfunction. Arch Dermatol. 2004;140(5):570
Conclusions: This case highlights the importance of recognizing and managing rare manifestations of widely used radioiodine contrasts, which may have been classified as allergic reactions/hives in the past.