Background:
Many interventions to improve transitions of care have been informed by patient concerns at the time of discharge, yet few studies have examined patient perceptions of factors that may have contributed to their readmission. Our objectives were to characterize patient‐centered readmission factors using structured survey responses and patients' own words.
Methods:
This is a prospective national study of readmitted patients at 13 hospitals across the United States participating in the Hospital Medicine Re‐engineering Network (HOMERUN). General medicine patients who were readmitted within 30 days participated in interviews with both quantitative (multiple‐choice) and qualitative (open‐ended) components. We analyzed quantitative data to identify the 5 most common factors among the domains in our survey: medication use, monitoring for danger signs, hospital contact information, transportation, basic needs (e.g., food and shelter), diet, social support, and substance abuse. To enhance our understanding of these factors, 2 investigators then independently coded qualitative data into themes, resolving discrepancies in coding through negotiated consensus.
Results:
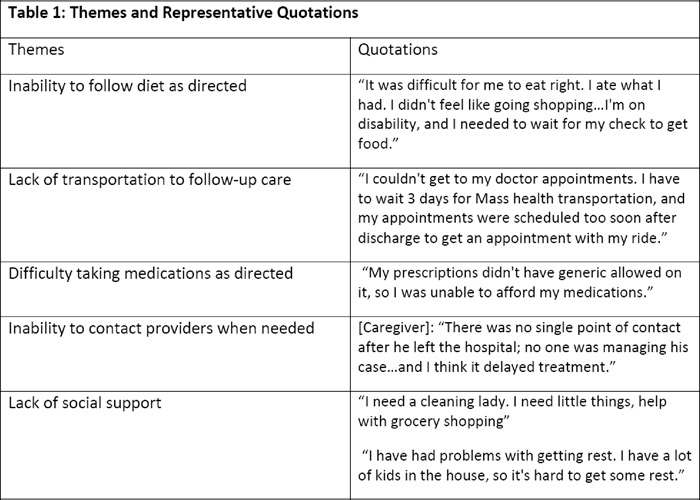
We analyzed results from 592 readmitted patients. The 5 most common factors patients cited as contributing to their readmission were: (1) inability to follow diet as directed (23%), (2) lack of transportation to follow‐up care (19.5%), (3) difficulty taking medications as directed (18%), (4) inability to contact providers when needed (14.5%), and (5) lack of social support (13%). We also identified themes and quotations from qualitative responses (Table 1) to better characterize these factors: (1) diet recommendations may be understood but access to recommended foods may limit adherence, (2) follow‐up appointments may create logistical challenges because they fail to account for patient's resources or preferences, (3) discharge medication regimen may be clear but issues with drug formularies and copays may prevent adherence, (4) hospital contact information may be clear but inability to reach someone familiar with the patient prevents meaningful exchanges, and (5) overall plans for care may be clear but lack of social support prevents adequate rest and accomplishing key daily tasks such as cooking, cleaning, or shopping.
Conclusions:
Readmitted patients identified several factors that may have contributed to their hospital readmission and explained ways that current transition care efforts fail to adequately address these factors. Tailoring discharge planning and postdischarge care to incorporate these patient‐centered concerns may improve the quality of discharge care and reduce readmissions.