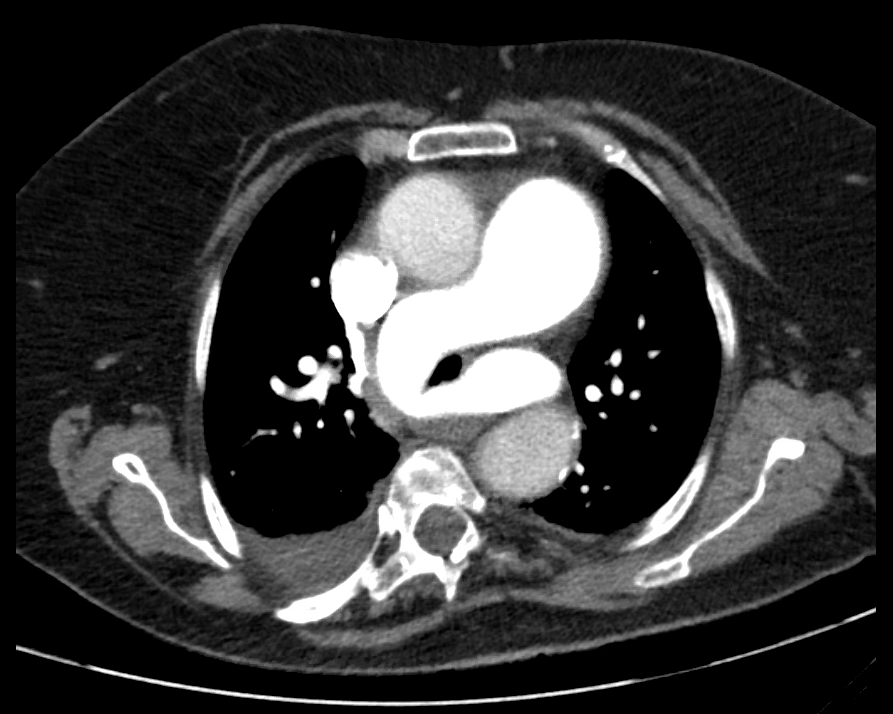
Case Presentation: 75-year-old female with past medical history of obesity (BMI 31.7 kg/m2), paroxysmal atrial fibrillation, hypertension, hypothyroidism, was admitted to the hospital for elective laparoscopic cholecystectomy. Patient tolerated the procedure without complications, however, post operatively, she was difficult to extubate due to hypercapnia of pCO2 of 100 mmHg in arterial blood gas. She was transferred to the surgical intensive care unit; her stay was complicated with an isolated episode of atrial fibrillation with rapid ventricular response which resolved with the use of beta blockers. Patient was successfully extubated 2 days after procedure, and was transferred to general medicine floors on post-op day 4 for management of atrial fibrillation. During hospitalization, the patient had several episodes of morning somnolence and occipital headaches which improved as the day progressed, morning venous blood gas analysis showed pCO2 of 95 and pH 7.21; additionally, patient experienced frequent episodes of hypoxia requiring supplemental oxygen, tachypnea, and tachycardia. Given her recent surgical procedure, episodes of tachycardia, and hypoxemia, she was deemed to have a moderate risk for pulmonary embolism based on Well’s Criteria, this prompted a CT angiogram of the chest. Result of the CT was significant for aneurysmal dilatation of the central pulmonary artery (PA) measuring 5 cm, and an anatomic variation of left pulmonary artery sling, with the left pulmonary artery arising from the posterior right pulmonary artery, coursing to the left behind the trachea and in front of the esophagus, narrowing the width of the trachea. Pulmonary medicine and thoracic surgery were consulted, patient was managed conservatively, and discharged with nocturnal BiPAP use.
Discussion: Pulmonary artery sling is a rare congenital vascular anomaly in which the left pulmonary artery originates from the right pulmonary artery and encircles the right main stem bronchus before entering the left lung, causing compression of the esophagus and trachea in severe cases. It is a condition mainly identified in infants in their first year of life, and presents as severe respiratory distress and or upper airway obstruction. Symptomatic infants require supportive therapy and surgical intervention to improve mortality. Asymptomatic patients will move into adolescence and adulthood; the diagnosis then is made as an incidental finding on imaging. Most patients described in the literature are children who presented early in their childhood, few cases are reported in adulthood; there are case reports of adolescents presenting with chest pain, and dyspnea on exertion. As there are no guidelines for the management of adults, the management is dependent on the practicing physician and the existing symptoms. Our patient presumptively became symptomatic after intubation, it is possible that the manipulation of the anatomy during the intubation process, triggered or worsened airway obstruction leading to difficulty in extubating and a recurrent morning hypercapnia, hypoxia, and tachypnea after extubation. On follow up, 8 weeks after hospitalization, patient was still requiring BiPAP for her morning symptoms.
Conclusions: This case illustrates an elderly patient with post-surgical hypercapnia, found to have a rare congenital vascular abnormality usually diagnosed during childhood.