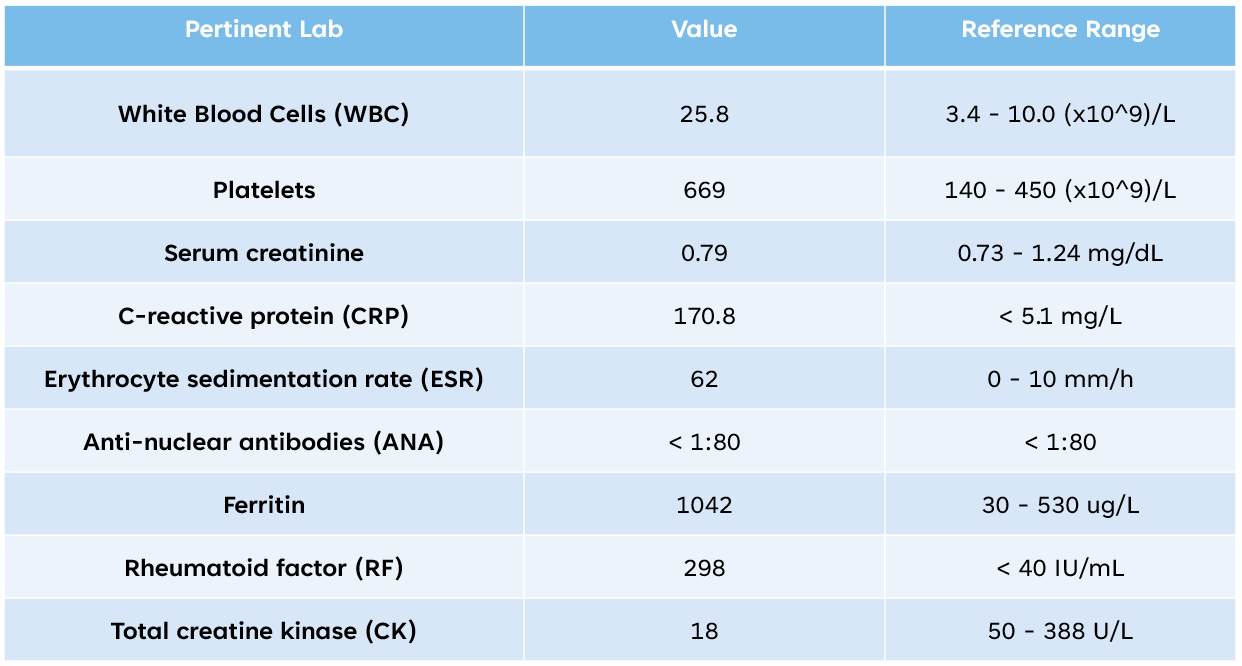
Case Presentation: An 80-year-old man with recently-diagnosed pulmonary fibrosis presented to the hospital with ascending bilateral lower extremity pain and weakness. His symptoms began in both feet and calves, and progressed proximally toward his thighs over the past 6 weeks. During this timeframe, his symptoms evolved from being able to ambulate for miles and climb stairs to being unable to walk without assistance due to exquisite pain. He endorsed intermittent fever, drenching night sweats, and unexpected weight loss but otherwise denied all other review of systems. Of note, he had two urgent care visits, with his symptoms speculated to be due to vascular claudicationHis initial vital signs were notable for a temperature of 100.8 °F. His lower extremities were warm, but had allodynia and hyperalgesia in bilateral thighs, calves, and dorsal surfaces of feet (right greater than left). He had 2+/2+ dorsalis pedis/anterior tibial pulses. His neurologic exam was remarkable for 3+/5 distal strength in bilateral ankles and feet (fluctuated due to pain), patellar reflexes 3+ and Achilles reflexes 2+ bilaterally. Pertinent labs from the patient’s initial serologic workup (table 1) were notable for leukocytosis, multiple elevated acute phase reactants, a negative ANA, and normal creatine kinase. Given the patient’s evidence of inflammation, the initial differential diagnosis focused on infectious, autoimmune, and neoplastic etiologies for his neuromuscular syndrome. Pertinent advanced imaging and CSF tests (figure 1) were notable for MRI of bilateral femurs with concordant EMG findings of intramuscular edema with myopathic changes. A muscle biopsy of the right vastus lateralis revealed necrotizing vasculitis and active/recent denervation. His final serologic workup was positive for myeloperoxidase antineutrophil cytoplasmic antibody (MPO-ANCA), confirming the diagnosis of ANCA-associated vasculitis with myopathy. The patient was started on induction systemic steroids and, eventually, transitioned to maintenance rituximab with significant improvement in his neuromuscular symptoms.
Discussion: ANCA-associated vasculitis (AAV) is a systemic condition often thought to affect the small vessels of the ears, lungs, kidneys, or brain. However, emerging literature in recent years has identified AAV with myopathy as a rare but important cause of subacute lower extremity muscle pain and weakness in hospitalized elderly patients. Clinician awareness is crucial as this condition is distinct from other myopathies, associated with unique complications and can result in neurologic disability if not treated early. When compared to inflammatory myositis or neuromuscular disorders, certain clinical features favor AAV with myopathy: initial distal > proximal symptoms, asymmetric distribution, predominant pain > weakness or fatigability, and a normal CK. Additionally, as observed in our patient, comorbid pulmonary fibrosis favors AAV as the etiology of a myopathy.
Conclusions: – In elderly patients presenting with subacute bilateral lower extremity pain or weakness, early consideration of AAV with myopathy as part of the differential diagnosis may prevent diagnostic and therapeutic delay in hospitalized patients. – AAV with myopathy can present with or without an elevated CK level, thus this single test can’t reliably rule in or rule out the disease. – Newly diagnosed pulmonary fibrosis warrants serologic evaluation for secondary causes, including connective tissue disorders.