Background: Acute Kidney Injury (AKI) is a common hospital problem which may lead to increased mortality, hospital costs, and increased length of stay (1). A leading cause of renal dysfunction in the inpatient population is drug nephrotoxicity. Several studies show that physician prescribers often do not take renal function into account with new or existing prescriptions, often leading to inappropriate dosing of renally cleared medications up to 50% of the time (2).
Purpose: Nephrotoxic alerts aimed at informing prescribing providers of acute kidney injury or baseline renal dysfunction have shown statistically significant improvement in changing prescriber habits (3). In particular, interruptive alerts informing providers of the development of AKI or CKD in patients can have a positive impact on careful use of nephrotoxic agents (4,5,6). A clinical decision support system specifically designed for non-steroidal anti inflammatory drugs (NSAID) ordering in the setting of all renal dysfunction, including CKD and AKI, has not been evaluated. We evaluated the use of a best practice alert (BPA) in NSAID ordering for patients with all cause renal dysfunction to determine impact on provider practice and incidence of AKI.
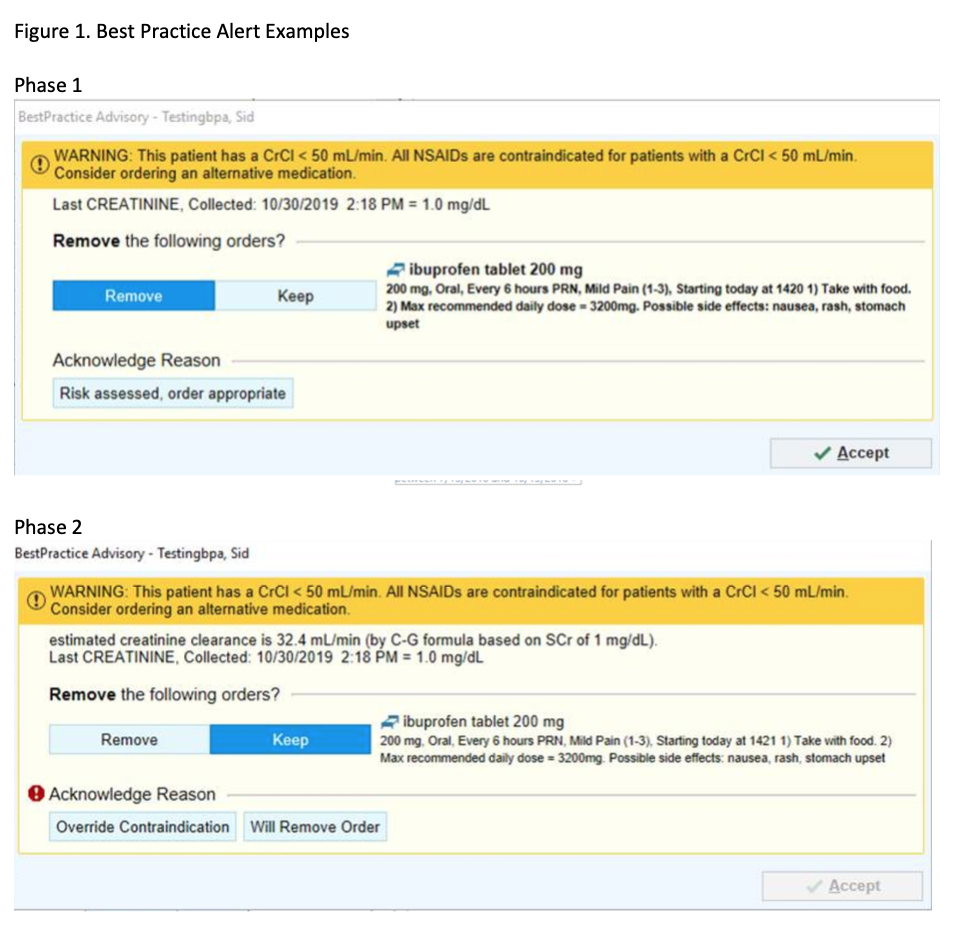
Description: The intervention was an interruptive alert in the EMR designed to alert the provider to renal dysfunction. We conducted a pre- post-study of this intervention in patients with documented pre-NSAID creatinine clearance less than 50 mL/min who received an NSAID order during hospitalization. Patients were adults (age >18) admitted to a large tertiary care hospital healthcare system. The phase 1 intervention (1/16/18-7/11/19) was a Best Practice Alert (BPA) triggered at the time of order entry when NSAID was ordered on a patient with a creatinine clearance <50 mL/min. Follow-up phase 2 intervention (7/12/19-10/31/19) was an update to the initial BPA including a display of the individual patient’s current creatinine clearance rather than creatinine alone and a change in override reason from “Risk assessed, order appropriate” to “Override contraindication”, as well as addition of “will remove order” button (Figure 1). We compared patient and provider characteristics between the three study periods, and compared the percentage of BPAs that were overridden by the provider between phases 1 and 2 of the BPA. Over 1,000 unique patients received a BPA in phase 1 after removal of duplicate BPA fires. 33% of orders were removed in total. In phase 2, the rate of removal was further increased (results ongoing). There was no difference between patients’ characteristics such as age and creatinine clearance. Overall, those patients with a CKD or HD flag had a higher rate of removal compared with acknowledgement. Duplicate orders were Home Meds had a lower rate of removal compared with acknowledgement.
Conclusions: Clinical Support Systems including Best Practice Alerts (BPAs) have been shown to be helpful in judicious use of nephrotoxic medicines for patients with renal dysfunction. Clinical support systems requiring an override may be more likely to affect provider management. Thus, Clinical Support Systems in the setting of NSAID ordering with renal dysfunction may be helpful in certain ordering provider and clinical patient populations.