Background: Hospital immobility is highly prevalent and known to cause various complications including deconditioning, pressure injuries, venous thromboembolism, readmissions and mortality(1). Due to the known consequences of immobility, there has been an increased emphasis on identifying patients at highest risk of immobilization and focusing efforts on maintaining function. Increasing patient mobilization has the potential to improve quality of care and hospital outcomes, including length of stay (LOS) and discharge disposition.
Purpose: Our goal and intervention are centered around an interdisciplinary and multifaceted approach that includes nursing documentation standardization with Activity Measure for Post-Acute Care (AM-PAC), addition of door posters/signs to clarify patient mobility status, and introduction of mobility games. Our aim is to utilize AM-PAC to identify patients at highest risk for prolonged length of stay and discharge to facility in order to best utilize our limited resources. We hypothesized that patients with stable or declining AM-PAC scores (based on initial and last AM-PAC) would be associated with longer LOS and higher percentage of discharge to facility.
Description: The first portion of this plan involves a hospital-wide preliminary analysis of inpatient mobility through initiation of AM-PAC documentation and assessment of outcomes of inpatients. We chose to evaluate all inpatient discharges from the months of July through September of 2023 at our tertiary care medical center. Our independent variable of interest is patient mobility measured by both the initial AM-PAC and delta AM-PACs (final minus initial) scores. The primary outcomes include discharge disposition and LOS.
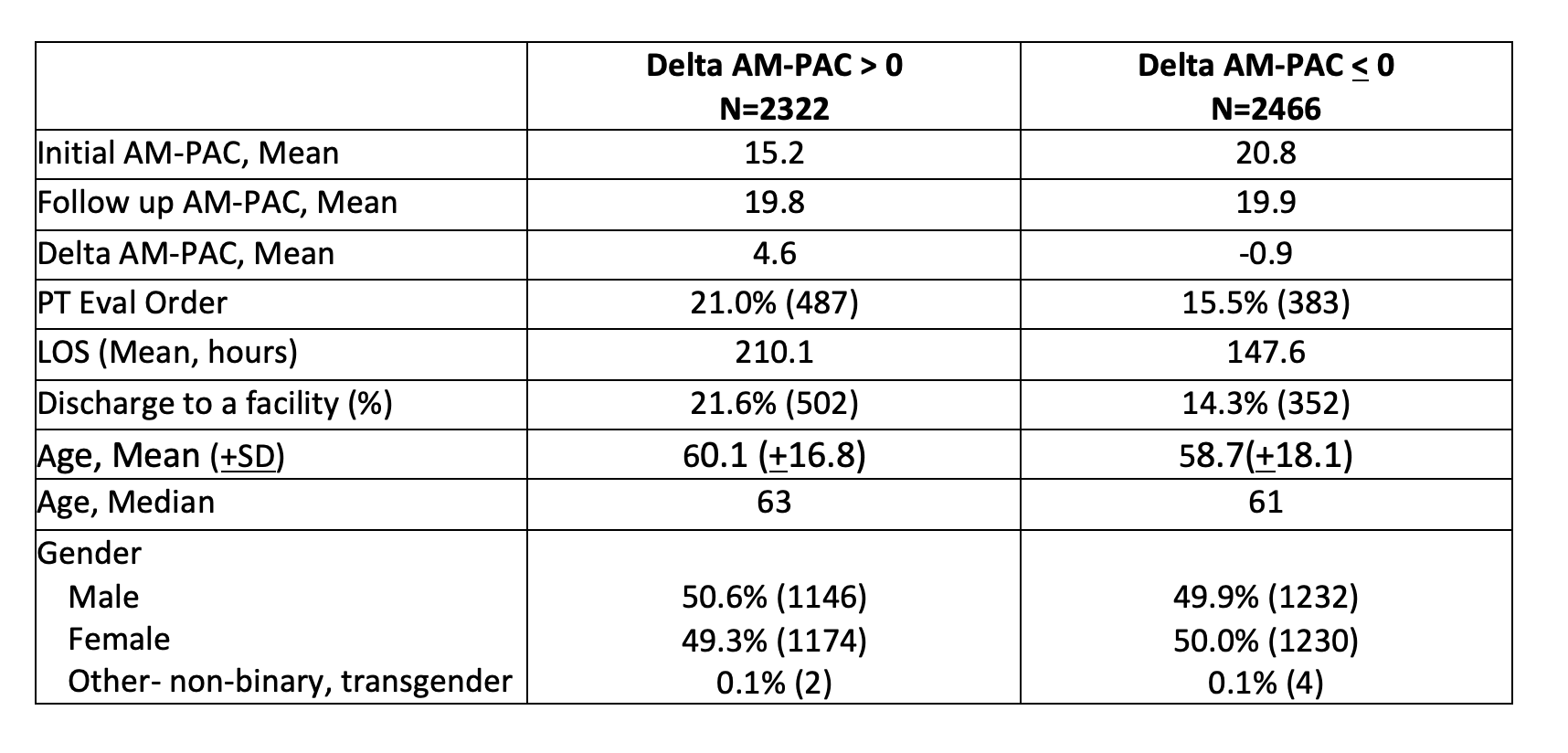
Conclusions: Our analysis revealed a total of 7792 discharges over the 3-month period. The percentage of patients with at least two AM-PAC scores was 61.4% (4788/7792). Of total patients 48.5% (2322/4788) had a delta AM-PAC >0 and 51.5% (2466/4788) had delta AM-PAC< 0. Of the patients with delta AM-PAC > 0, 21.6% (502/2322) were discharged to a facility compared to 14.3% (352/2466) with delta AM-PAC < 0 (Table 1). Interestingly, our results were contrary to our hypothesis. Patients with delta AM-PAC< 0 had shorter length of stays and lower rates of discharge to facility. We identified several reasons for these results and performed further analysis to better understand our unexpected results (Table 1). We conclude that delta AM-PAC is not the best tool to predict hospital outcomes and instead we should assess other process measures. Future directions include evaluating the utility of initial AM-PAC score as a predictor of patient outcome. Preliminary logistic regression models controlling for demographics and primary diagnosis appear to show 20% lower odds of discharge to a facility for every point increase in initial AM-PAC (OR 0.802, 95%CI 0.788-0.816). This project is ongoing and will continue through Spring of 2024.