Background: Peripherally inserted central catheters (PICCs) are an increasingly popular choice in the acute care setting for intravenous therapy. However, compared to other catheters, PICCs are associated with a higher risk for venous thromboembolism and blood stream infection, with multi-lumen PICCs having higher complication rates than single lumen. Midline catheters are associated with a much lower risk for complications compared to PICCs and can be a sound alternative. The decision making process for selection between PICC and midline catheters can be challenging. A multidisciplinary panel at our multi-entity academic healthcare system developed a set of evidence-based recommendations to support provider decision-making for PICC and midline use, which were then implemented as a point-of-care clinical decision support (CDS) tool in an electronic health record (Sunrise Clinical Manager 5.0, Allscripts, Chicago, IL). This CDS led providers through a set of questions and displayed relevant clinical patient data (Figure 1). The recommended catheter was pre-selected by the CDS tool, but providers could override if necessary.
Methods: : Impact of this evidence-based PICC/Midline CDS tool on provider ordering was evaluated using a pre-test/post–test study design (study timeframe: 11/1/2012 to 8/1/2015, divided into three study period). Mixed effects regression models were used as the primary analysis to account for provider correlated ordering data. Two outcomes were evaluated: (1) proportion of PICC orders placed (defined as PICC orders /PICC+midline orders) and (2) proportion of double-lumen PICC orders placed (defined as double-lumen PICC orders /all PICC orders).
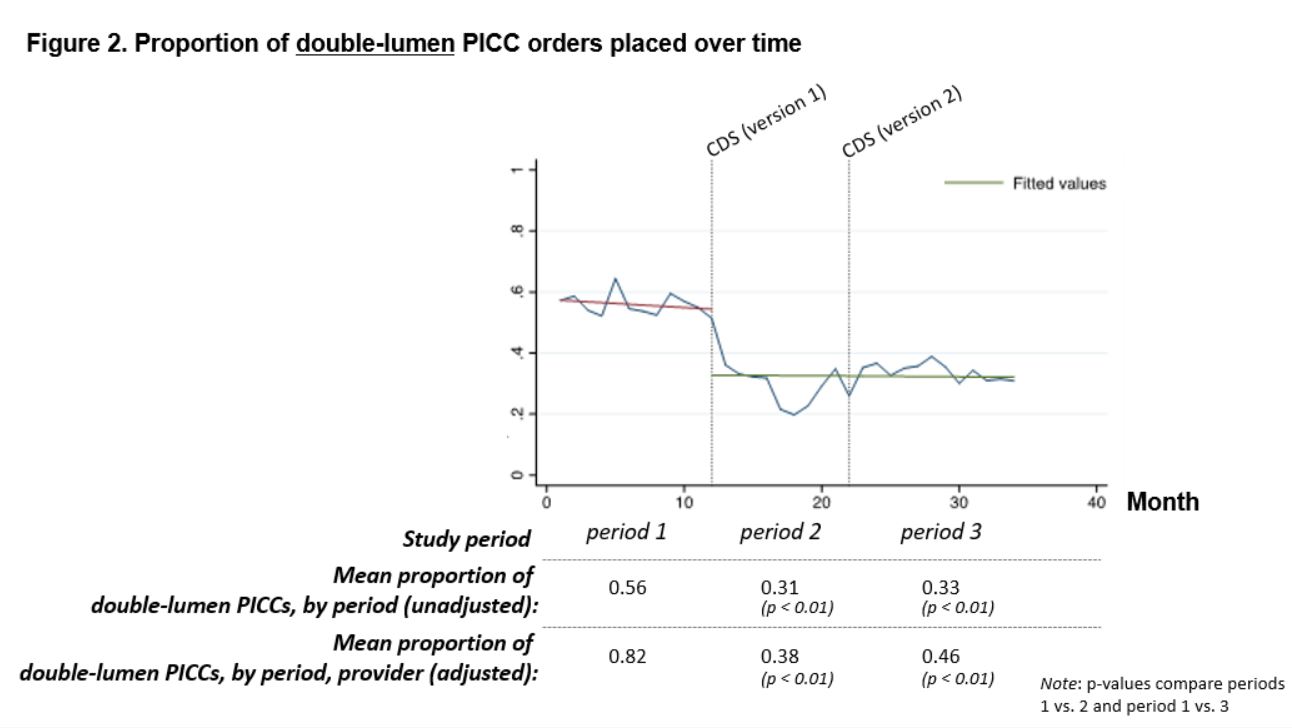
Results: 7,391 patients had a PICC or midline catheter order placed (12.2% of all admissions). For outcome one, adjusted results suggested no statistically significant difference between the pre and post-intervention periods. For outcome two, analysis suggested a large statistically significant decrease in the proportion of double-lumen PICC orders (Figure 2).
Conclusions: Although results suggest a minimal impact of the CDS tool on the proportion of PICC orders placed by providers, the tool resulted in a significant decrease in double-lumen PICC orders, suggesting the evidence against double-lumen PICC use may have been less familiar to providers. The CDS interface design likely had a significant impact on this outcome, as the tool defaulted to a single-lumen PICC order unless otherwise indicated. Results suggest that when CDS tools are designed using factors that positively affect outcomes (e.g. stakeholder involvement, integration into clinician workflow, recommendations for action, use of defaults), they can be an effective means for integrating evidence at the point of care and can change practice.
.jpg)