Background: In order to reduce overuse, many hospitals have conducted studies and implemented protocols with the goal of reducing non-indicated telemetry monitoring. A common tool that institutions utilize for these changes are the clinical decision support systems (CDSS). In this report, we will present the telemetry protocol utilized by our hospital and review its effects on telemetry overuse. Huntington Hospital is a 625-bed community and teaching center located in Pasadena, California. It is composed of healthcare providers ranging from resident physicians to multiple hospitalist groups.
Methods: An analysis of data for patients on telemetry was conducted 6 months pre-implementation and 12 months after the launch of the electronic alert (post-implementation). This analysis was conducted for each of the four data sets: 1) patients managed by residents with telemetry used >2 days, 2) patients managed by residents with any telemetry, 3) patients managed by all physicians with telemetry used >2 days, and 4) patients managed by all physicians with any telemetry. We excluded patients in the intensive care unit, emergency department, operating room, post anesthesia care unit, and step down unit. We also excluded patients with DRGs for which telemetry was indicated according to recommendations from the ACC/AHA guidelines. During this period, a total of 24,276 patient hospitalizations were reviewed: 14,347 patients in 2018 and 9,929 patients in 2019.
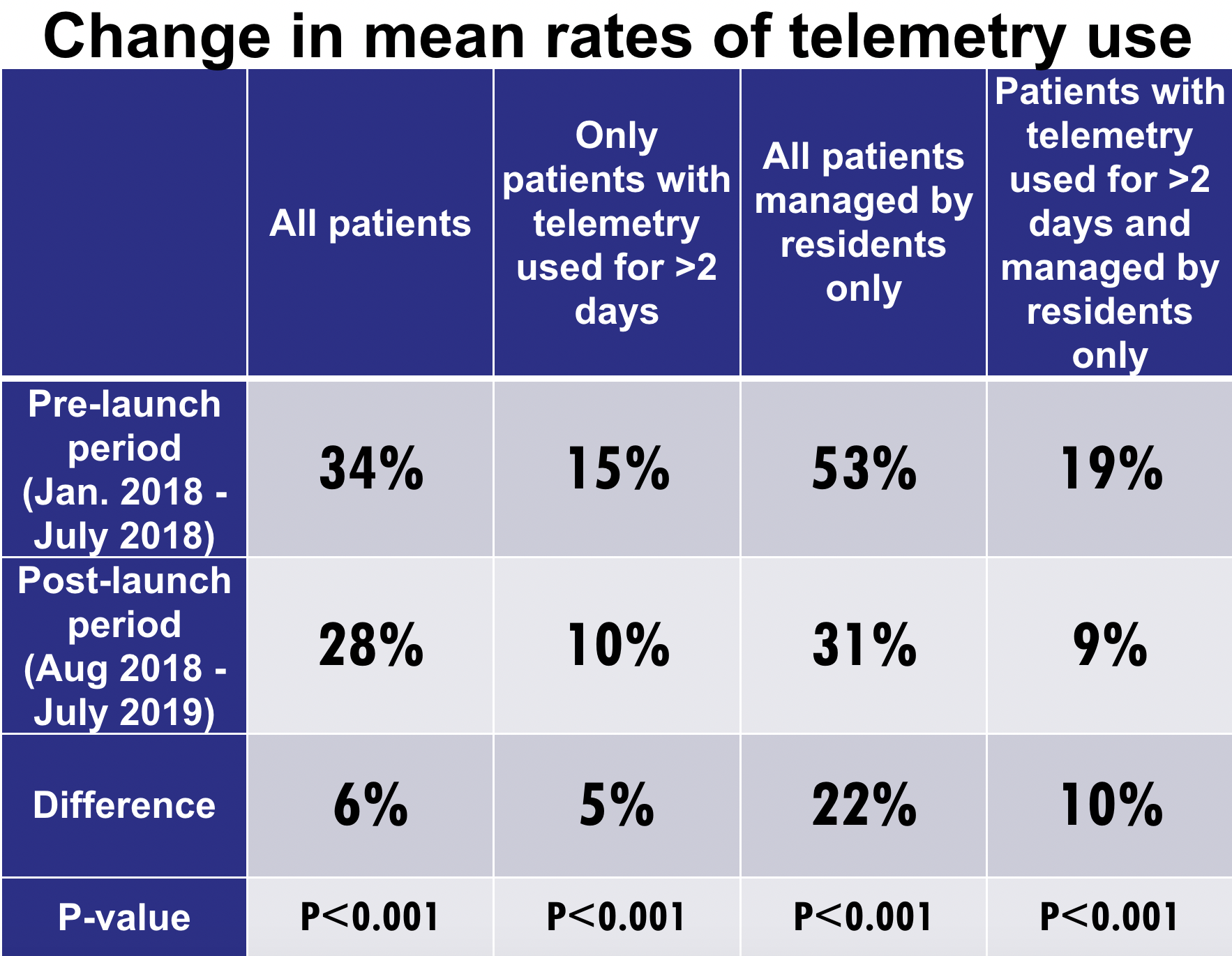
Results: The mean rates of telemetry use for all reviewed patient hospitalizations (managed by all physicians) in the pre-implementation period was 34%. This was reduced to 28% following the implementation of the electronic alert system, resulting in an overall 6% reduction in mean telemetry use (p<0.001). Furthermore, there were also witnessed reductions in mean rates of telemetry use for the other 3 groups that we analyzed.
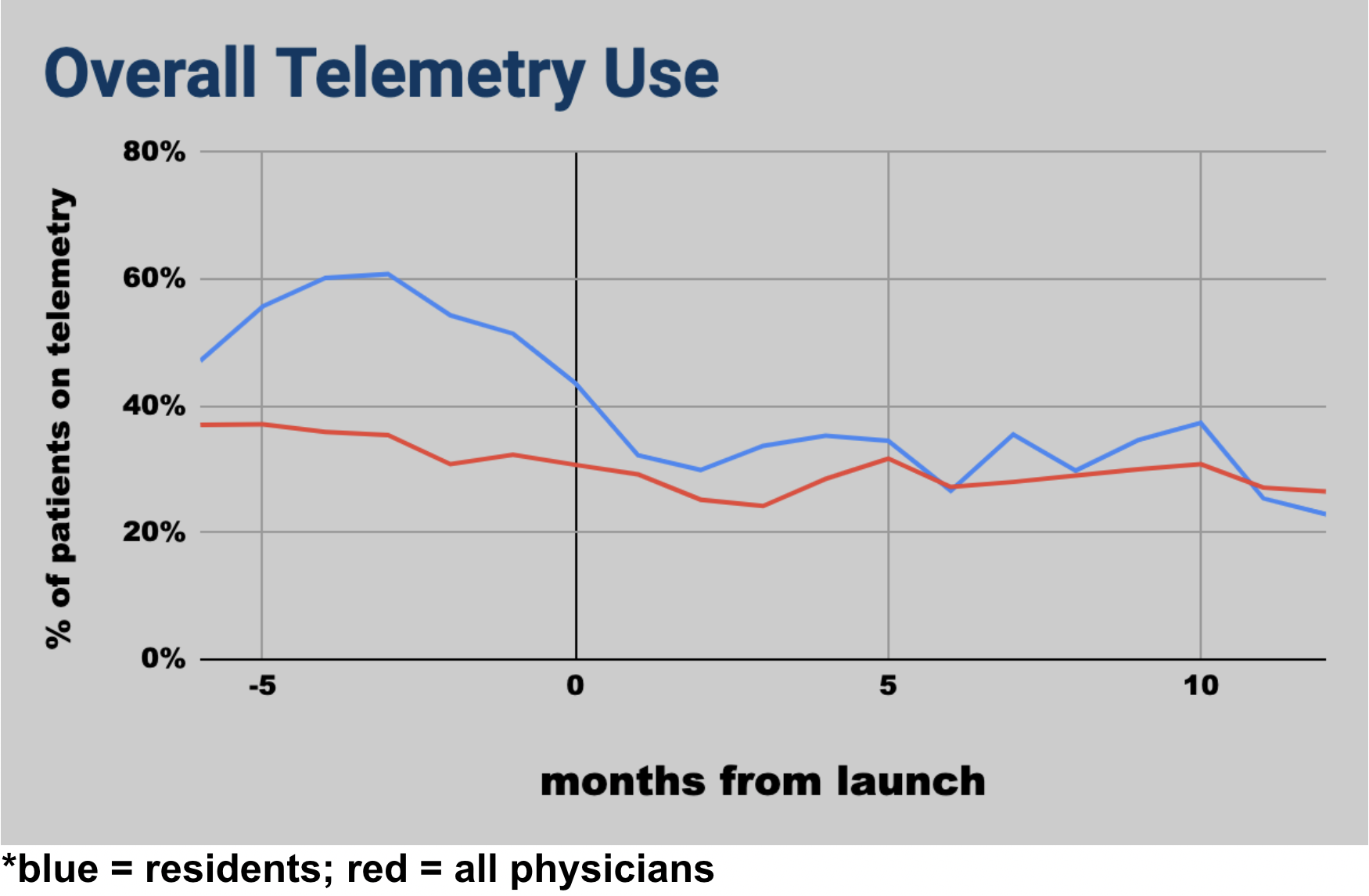
Conclusions: The implementation of a passive electronic alert built into the EMR system reduced the overall rate of telemetry overuse at our institution by 6% between the two time periods that we studied. Telemetry use rates in patients managed by residents reduced by 22% in this period, suggesting an added educational value of our alert system. The limitations of this report include the short follow-up period of 12 months. From our time-bound analysis, we will be unable to demonstrate if this reduction in telemetry overuse can persist into the active implementation phase or even beyond. Another limitation is the setting of a single center study in a community teaching hospital. Although CDSS is a powerful tool for guiding changes in practice, the limitations of CDSS itself cannot be ignored. Similar to telemetry alarm fatigue, there can be electronic alert fatigue which can affect clinician response. The fact that the alerts pop-up on the center of the screen at the very moment the clinical decision is made can really disrupt the workflow of clinicians. This may explain the slight increase in telemetry usage rates a few months post-implementation. One possible solution is to place the telemetry alerts in a side-bar or “to-do-list” much like our current EHR’s documentation query system, but further exploration is needed. An important factor to keep in mind moving forward is not to compromise patient care or safety with these changes. Future studies can look at the changes in volume of emergency codes and rapid responses with lower rates of telemetry use. Along the same vein, patient satisfaction can also be studied as it may be influenced by excessive telemetry use.