Background: Academic medical centers with teaching and non-teaching teams and complex call schedules frequently utilize triage providers to allocate admissions to each inpatient service. In this process, the ED provider hands off the patient to a triage provider, who then hands off the patient to the admitting provider. This sequential handoff can lead to decay of information and communication errors.
Methods: To study the effect of the sequential handoff system using a triage provider, we conducted a cross-sectional survey at a 550-bed academic medical center. Those eligible for the survey included faculty, advance practice providers and residents from both Emergency Medicine and Internal Medicine. Survey questions addressed the safety and efficiency of the handoff system and the quality of communication between the providers. The respondents indicated their responses via a 9-point Likert scale and an open-ended question about the patient admission process.
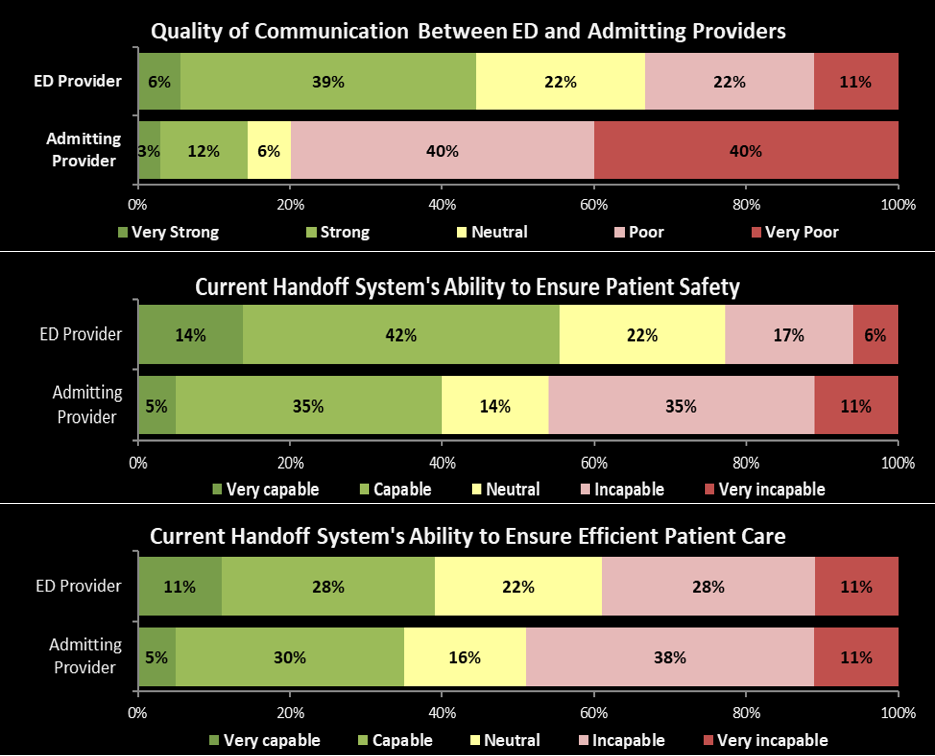
Results: Response rates were 41% for ED providers (39/96) and 27% for admitting providers (50/187). Overall, 32% of all respondents rated the quality of communication as “strong” or “very strong”. Compared to admitting providers, the ED providers reported much higher quality of communications (p-value <0.001). 45% of the ED providers found the quality of communication with the inpatient providers to be either “very strong” or “strong.” Only 15% of the inpatient providers found the quality of communication with the ED providers to be “very strong” or “strong.”
When evaluating the capability of the current handoff system’s ability to ensure patient safety, 56% of ED providers and 40% of admitting providers found the system to be “very capable” or “capable.” 39% percent of ED providers and 35% of admitting providers found the current handoff system’s ability to ensure efficient patient care to be either “very capable” or “capable.”
Some common themes among the open-ended question about the admission process include frustrations with the “middle man” and the desire to communicate directly with the other providers. One respondent felt a better communication system could “save time, allow for better patient care and prevent errors in a timely fashion.”
Conclusions: The perception of the quality of communication of the sequential handoff system was significantly worse among the inpatient providers. This difference suggests providers who function downstream of a sequential handoff are more likely to be aware of decay of information and resulting errors. We have adjusted our handoff process to remove the triage provider from the flow of clinical information and we plan to study how the change to a direct handoff affects the quality, safety, and efficiency of this critical process.
.png)
