Background: The Society of Hospital Medicine (SHM) identifies repetitive CBC & chemistry testing as low-value, and they selected this as a Choosing Wisely Recommendation. Overuse of phlebotomy is associated with hospital-acquired anemia, decreased patient satisfaction and increased hospital costs. Process improvement techniques have been utilized to reduce inpatient phlebotomy, but prospectively identifying a cohort of stable patients has been a challenge. The Veterans Health Administration (VHA) utilizes a National Utilization Management Integration (NUMI) database to track patients’ level of care for utilization review. Patients identified in NUMI with a recommended level of care (RLOC) of waiting for placement were deemed to be a suitable cohort for a laboratory reduction project.
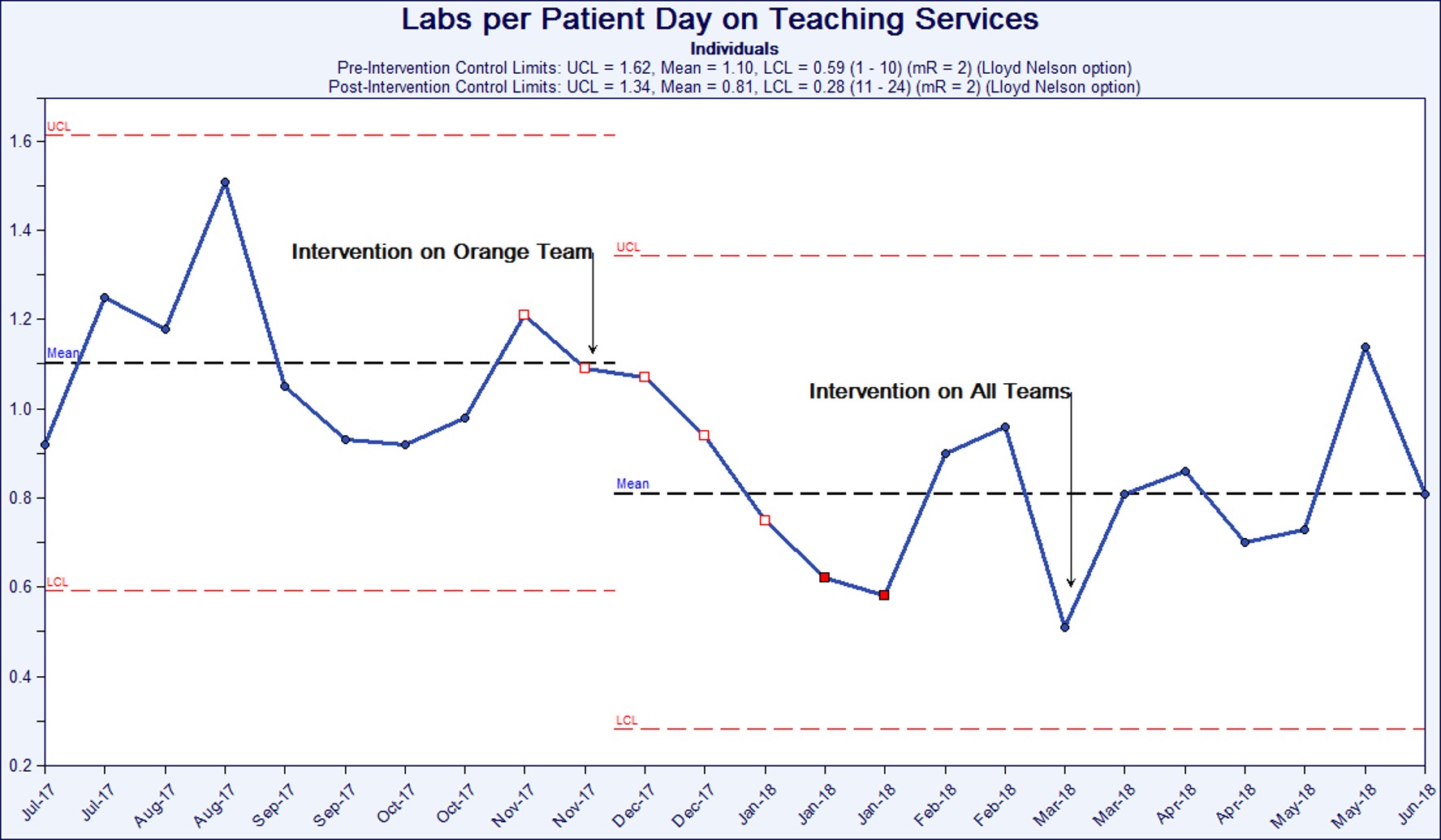
Methods: A global aim of reduction of 0.25 labs per patient day for the intervention period was selected. The NUMI database identified patients with a RLOC of community living center (CLC), skilled nursing facility (SNF), inpatient rehabilitation or hospice for each two-week block of the 2017-2018 academic year. From November 2017 through June 2018, a physician team presented a short didactic session to one inpatient teaching team at the Louis Stokes Cleveland Veterans Affairs Medical Center (LSCVAMC). In March of 2018, all inpatient teaching medical services at LSCVAMC were included in the educational intervention. Risks of hospital acquired anemia and the SHM’s Choosing Wisely phlebotomy recommendation were discussed. Residents were encouraged to discuss laboratory orders during attending rounds and to document this discussion. A summary visual aid was posted on all order-entry computers in the team room. Labs per patient-day for patients with the above RLOC in NUMI were monitored on inpatient teaching services for 18 weeks of baseline data plus the 30-week intervention period and were graphed using control charts.
Results: Labs per patient day decreased significantly from a baseline mean of 1.10 labs per patient day to 0.81 by the end of the intervention period (One Tailed T-Test, p < 0.005). For 24 consecutive weeks post-intervention, labs per patient day fell below the pre-intervention mean, indicating a statistically significant shift. The first block when the intervention was applied to all teaching services, special cause variation was observed, as labs were reduced to 0.51 labs per patient day.
Conclusions: The educational intervention was effective at achieving and sustaining the aim of a reduction by 0.25 labs per patient day in patients whose RLOC identified by NUMI as CLC, SNF, rehabilitation or hospice. This reduction met statistical significance by One Tailed T-test. Results before intervention were in statistical control, suggesting a stable process. After a post-intervention shift, the results remained in control, confirming sustained results. Furthermore special cause variation was observed during the intervention period. This patient group thus represents a cohort for future interventions to reduce repetitive phlebotomy. Furthermore, this identifies the VHA’s NUMI system as a process improvement tool for hospitalists.