Background: Guidelines suggest venous thromboembolism risk stratification, and against use of prophylaxis in low risk medically ill hospitalized patients. Our hospital did not have a formal risk stratification process embedded into the electronic medical record (EMR) for provider use, and therefore it was common practice to administer pharmacologic prophylaxis to most medically ill patients regardless of risk. Prior rates of administration for low-risk hospitalized patients were identified through involvement in a statewide continuous quality improvement collaborative. In October 2018, we incorporated the 4-factor IMPROVE validated score calculator into the EMR admission order process with the intention of decreasing pharmacologic prophylaxis administration to low-risk patients while maintaining use in high-risk patients. The new order process proved cumbersome, and obstructive to workflow for admitting providers. We hypothesized that the total rate of pharmacologic prophylaxis ordered by hospital day 1 was reduced after implementation of this new system, with associated reduction of VTE pharmacologic prophylaxis administration to both low-risk and high-risk patients.
Methods: We performed a retrospective review and comparative analysis of patients admitted to adult general practice units for a non-surgical condition before and after implementation of the VTE prophylaxis order process. Baseline pre-implementation prophylaxis rates were obtained from existing retrospective data from a state-wide continuous quality collaborative. Post-implementation data was retrospectively obtained from chart abstraction. Our primary end-point was VTE prophylaxis administration rates pre- and post- implementation of the order system. Secondary evaluation included provider use of the order system on admission, and the impact on rates of VTE prophylaxis throughout patients’ hospitalization.
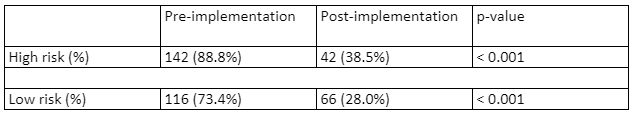
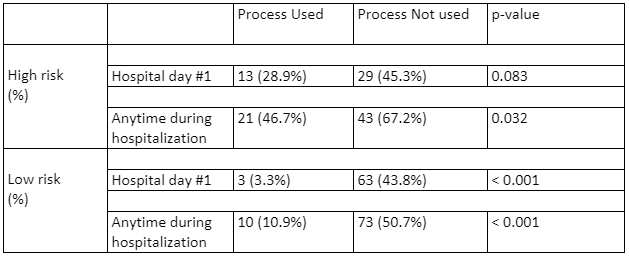
Results: With implementation of the order process into our EMR, rate of VTE prophylaxis administration to low-risk patients by hospital day 1 fell from 73.4% to 28.0% (p<0.001). Despite this intended reduction, there was a concomitant drop in prophylaxis administration to high-risk patients from 88.8% to 38.5% (p<0.001). Table 1 highlights this drop in prophylaxis administration pre- and post- implementation of the VTE order process. As highlighted in table 2, high-risk patients received VTE prophylaxis by hospital day #1 at a rate of 28.9% when admitting providers used the VTE order process, as compared to 45.3% without use, resulting in a 16.4% difference in prophylaxis coverage rate, with trend toward statistical significance (p=0.083). This reduced rate of coverage persisted throughout the hospitalization with statistical significance, as shown in Table 2. Conversely, low-risk patients received VTE prophylaxis at a rate of 3.3% when admitted using the VTE order process, as compared to 43.8% without use (p<0.001), with similar persistence throughout hospitalization (Table 2).
Conclusions: Implementation of an order process into the EMR for inpatient management of VTE prophylaxis has demonstrated promise, with unintended consequences. The system was effective in reducing rate of VTE prophylaxis administration to low-risk patients, however adjustments in work-flow are needed to maintain appropriate coverage rate for high-risk patients.