Background: Telemetry over utilization increases wasted spending, increases alarm fatigue, and creates patient safety risks. Despite the presence of American Heart Association (AHA) practice guidelines, patients are often placed on telemetry for inappropriate reasons at the discretion of the medical provider and are monitored for longer than anticipated. The goal of this quality improvement project was to decrease inappropriate telemetry utilization by updating the electronic telemetry order to incorporate the 2017 AHA practice guidelines on appropriate usage of telemetry and by using an electronic nursing screening task form to safely discontinue patients from telemetry when it is no longer indicated. The process change was implemented at four major hospitals within the Emory Healthcare system including Emory University Hospital (EUH), Emory University Hospital Midtown (EUHM), Emory Johns Creek Hospital (EJCH), and Emory Saint Joseph’s Hospital (ESJH). The electronic order was changed to incorporate evidence-based indications for use of telemetry according to the AHA telemetry practice guidelines. These indications are automatically linked to a duration of monitoring of 36 hours, 72 hours, or continuous. An electronic nursing screening task form is used to discontinue telemetry. If the patient is deemed to be safe to be removed from telemetry, the order for telemetry is automatically discontinued and the nurse notifies the provider regarding the discontinuation of telemetry. If the screening indicates a need for ongoing cardiac monitoring, the patient remains on telemetry and the order continues to be active. Re-screening with the task form occurs in 24 hour intervals after the initial selected duration.
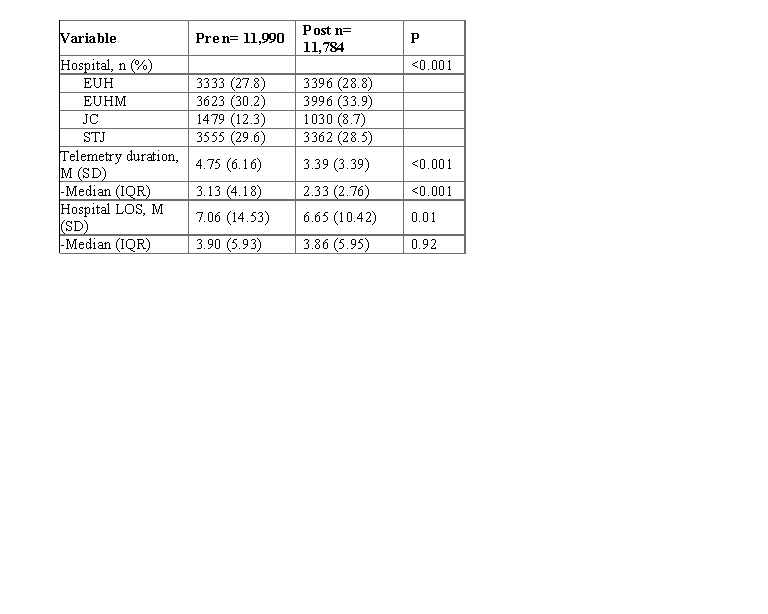
Methods: A retrospective analysis was done to evaluate the change in telemetry utilization before and after the telemetry protocol was implemented. The average and median number of days of telemetry monitoring was compared during the pre- (January – June 2018) and post-intervention (April – September 2019) periods. IRB approval was obtained. Data for telemetry length of monitoring and hospital length of stay was collected from the data warehouse on all adult patients with telemetry order admitted under inpatient and observation status at all four hospitals.
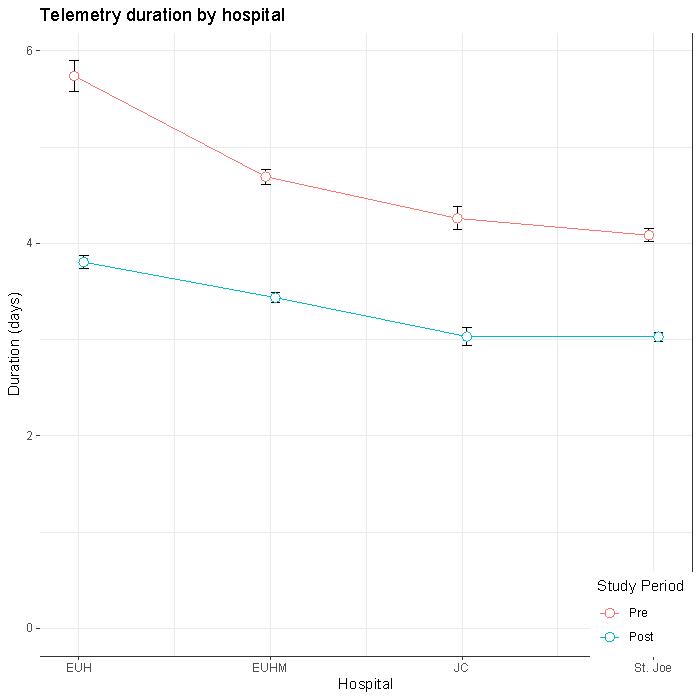
Results: There were a total of 23,774 encounters with telemetry duration and hospital length of stay (LOS). Of these encounters, 50.4% occurred before the intervention and 49.6% occurred post-intervention. Using a chi-square test, the distribution of telemetry encounters by hospital significantly differed between pre- and post- periods (p <0.001). The average telemetry duration in the post-intervention period was found to be 3.4 days compared to average duration of 4.8 days in pre-intervention period (p<0.001). Additionally, the post-intervention encounters had significantly shorter hospital stays (6.7 vs 7.1 days, p=0.01).
Conclusions: The results of our study demonstrate a statistically significant decrease in overall duration of telemetry monitoring in hospital patients by nearly 1.5 days with the implementation of a multi-factorial protocol by hard-wiring the AHA practice guidelines into the electronic ordering system and utilizing a nursing discontinuation protocol for telemetry. The approximate cost of delivering telemetry monitoring at our hospital system is $34/day per patient. Our results show a cost avoidance of approximately $504,000 across the hospital system during this 6 month period.