Background: There is a paucity of literature examining length of stay for medical patients requiring discharge to subacute rehabilitation facilities (SAR). At our institution, this subset of patients had an average length of stay (ALOS) of 8.2 days while medical patients being discharged to home had ALOS of 4.2 days during the first half of 2018. We also noticed an increase in unnecessary physical therapy consults. These were ordered on admission when many patients were too ill to be assessed or were already at their baseline. Furthermore, the therapist’s recommendation was at times discordant with the patient’s wishes and/or ability. This led to more time spent planning discharge, an increase in ALOS and suboptimal use of resources. These challenges were amplified on Unit 4900 due to its large size (41 beds).We aimed to improve triage and collaboratively discuss each case in a way that would lead to a more efficient and patient-centered discharge plans.
Methods: Our existing workflow involved twice daily interdisciplinary huddles as a forum to discuss safety, clinical updates, disposition planning, and barriers to discharge. We added a single physical therapist to both huddles on Unit 4900.At these huddles, we would identify patients who had new therapy orders and discuss their functional baseline, potential for improvement, and medical readiness for assessment. We would discuss evaluations completed since the previous huddle. The therapist would recommend how many hours of therapy the patient could tolerate (e.g. 0.5, 1.5, or over 3). We would then come to a team-based consensus regarding appropriate disposition based on the patient’s wishes and ability.Because patients discharged to SAR require the most planning and have a longer ALOS, we identified length of stay for this group as the best measure. The change was initiated September, 2018. Expecting to have a gradual wash-in period of a month, we evaluated ALOS for medical patients in the four months prior and the four months after.
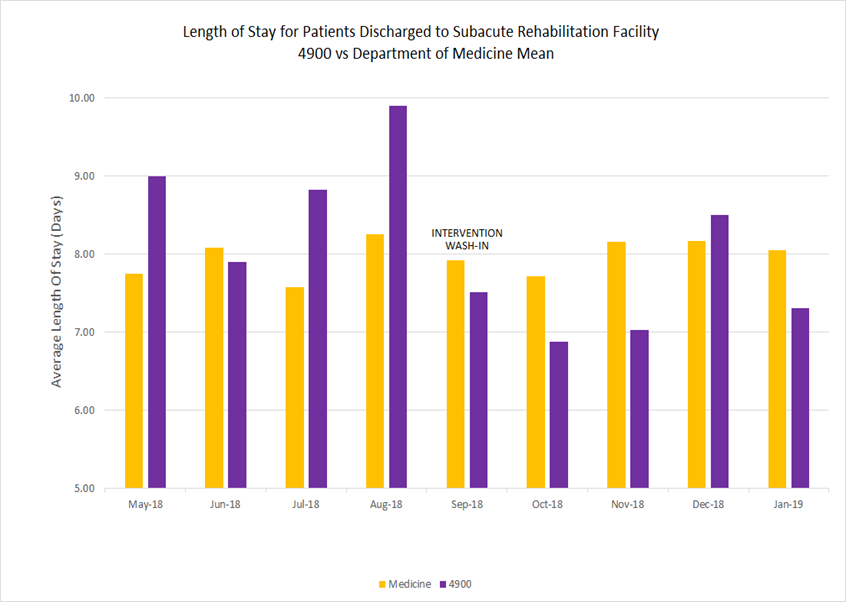
Results: The overall average length of stay for all medical patients being discharged to a subacute facility from the institution was consistent at approximately 8 days during the study period. Prior to intervention, Unit 4900 was frequently above this mean.While we expected a wash-in period as teams acclimated to the change in workflow, an immediate and dramatic improvement in ALOS was noted as soon as the intervention was made. The spike noted in December was due to several outlier patients with hospital stays of over 40 days being discharged. Despite this, the unit’s ALOS fell from approximately 9 days pre-intervention to 7.5 days post-intervention. (See graph)
Conclusions: The inclusion of a physical therapist in interdisciplinary huddles with collaborative discussion regarding management resulted in a dramatic improvement in ALOS for patients being discharged to SAR. Collaborative triage allowed therapists to focus in a more meaningful way on patients who were medically ready and would have a benefit from evaluation. After assessment, another team-based discussion helped facilitate getting each patient to his or her most desired and feasible disposition. Prior to intervention, these efforts were fragmented and often led to discharge plans that were less desirable or even impossible for the patient, requiring subsequent alteration which led to avoidable inpatient days.We propose the permanent addition of dedicated PT staff to unit based interdisciplinary huddles would have ongoing impact.