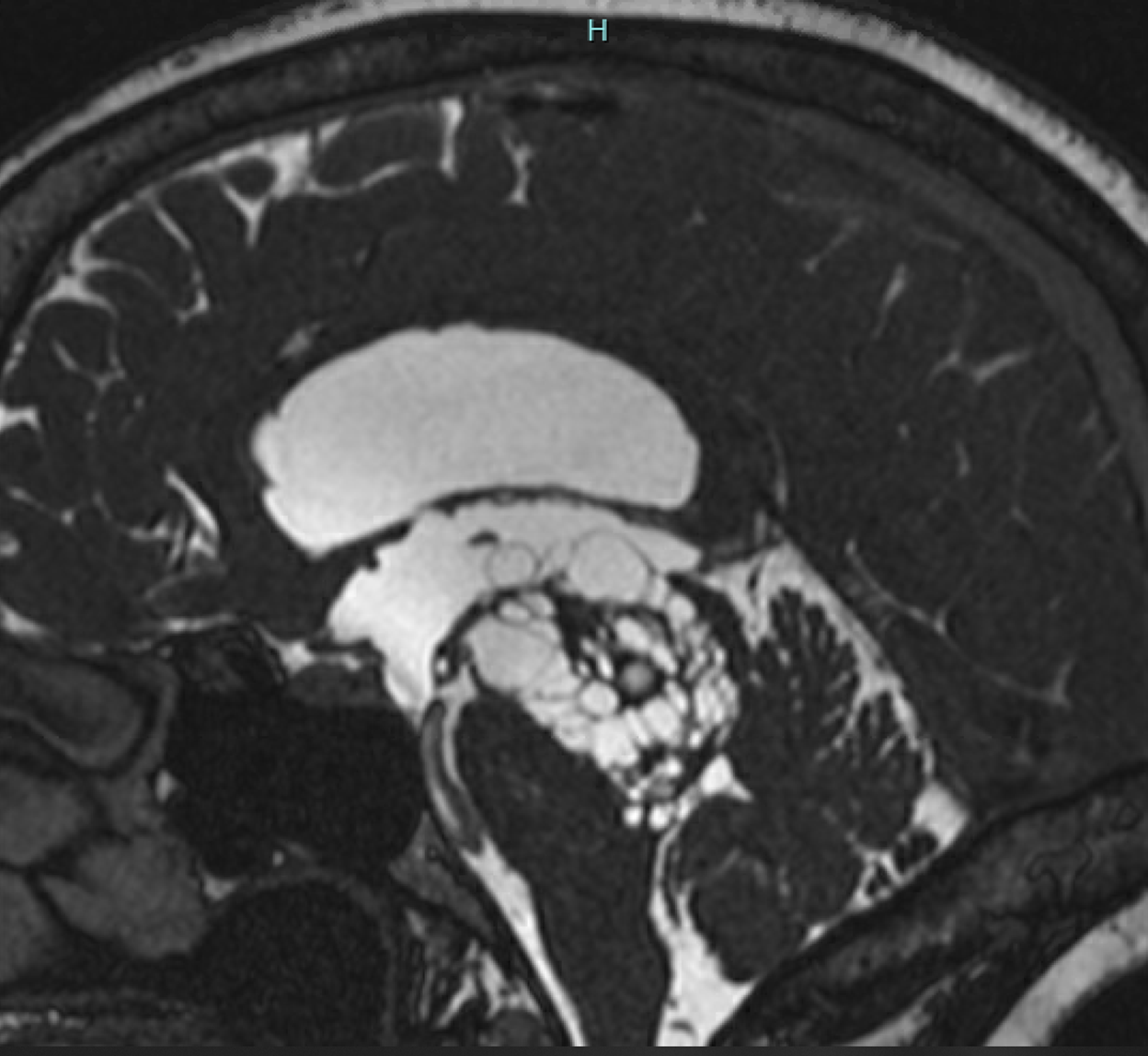
Case Presentation: A 58-year-old female presented to the emergency department after a lower lip laceration from slipping in her bathtub. She has a history of chronic trigeminal neuralgia and is now complaining of progressive weakness, imbalance over the past year, memory loss, and urinary incontinence for the past two days. On exam, the patient was afebrile, blood pressure 154mmHg/89mmHg, and heart rate 87 beats per minute. Neurologic exam revealed spasticity of her bilateral lower limbs, worse with her right leg, and hyperesthesia of her left face in the V2 and V3 distribution, which was consistent with trigeminal neuralgia. Additionally, her stance was widely spaced and unstable. A computerized tomography (CT) head which showed evidence of ventriculomegaly with a complex appearing multicystic lesion adjacent to the third and fourth ventricles. A magnetic resonance imaging (MRI) head Stealth with Cineflow redemonstrated the multicystic midline mass involving the upper pons, midbrain, bilateral thalami, and left hippocampus, consistent with a giant tumefactive perivascular spaces (Images). These lesions caused severe compression of the cerebral aqueduct resulting in obstructive hydrocephalus of the third and lateral ventricles. Due to lack of evidence of cerebrospinal fluid (CSF) flow through the cerebral aqueduct on the cineflow images, a ventriculoperitoneal (VP) shunt was recommended by neurosurgery. Patient underwent shunt placement for CSF diversion, with an improvement in gait within one week of surgery. She was discharged and followed up in two weeks and three months to monitor her progress and function of the VP shunt with non-contrast CT for shunt series.
Discussion: Perivascular spaces also known as Virchow-Robin spaces are normal interstitial fluid-filled structures that accompany arteries and arterioles as they penetrate the brain, typically less than 2mm in diameter. Rarely, these spaces can dilate into multi-cystic masses. The phenomenon is known as giant tumefactive perivascular spaces. There have been 37 such cases reported in literature since 1988.Characteristics of perivascular spaces include round or oval, single or multilocular lesions that are isointense relative to CSF. Depending on the location, size, and mass effect these lesions can cause a variety of symptoms. Of the 37 cases reported in literature, approximately 50% of patients presented with headache. Other related symptoms include dizziness, dementia, visual changes, post-trauma, seizure, syncope, memory problems, poor balance, and poor concentration. Nine of 37 cases had associated hydrocephalus, and of those patients three had a VP shunt placed, five patients had a ventriculostomy, and one patient had cystoperitoneal shunting.As for this patient, the location of her giant tumefactive perivascular space caused severe compression and stenosis of the cerebral aqueduct. That resulted in obstructive hydrocephalus, the likely explanation for her symptoms of progressive weakness, imbalance, memory loss, and urinary incontinence. Additionally, the involvement of the pontine area could explain compression of her trigeminal nerve causing trigeminal neuralgia.
Conclusions: Since giant tumefactive perivascular spaces are rare and can often be mistaken for other pathologic processes like a cystic neoplasm, parasitic cysts, ventricular diverticula, cystic infarction, or non-neoplastic neuroepithelial cysts, it is important for hospitalists to recognize such lesions to avoid unnecessary workup like a brain biopsy.