Background: Asking patients “what matters” to them is one of the 4 evidence-based elements of care developed by the Age-Friendly Health Systems initiative to improve the care of older adults, and the question “what matters most” has been extended to other settings. We conducted a study to assess the frequency and categories of responses to this question in patients hospitalized on a general medicine unit.
Methods: The study was based on two acute care general medicine units in a 600-bed tertiary care teaching hospital. Over a 1 month period, hospitalized patients were identified for potential participation by reviewing daily patient lists, and excluded if they had delirium, end-stage dementia, or were noted by staff to have active interpersonal conflict. Interpreters were used when needed for patients with limited English proficiency. Study staff approached patients on consecutive weekdays and invited them to complete a brief interview, recording the answers to “What matters most to you today?” and, later in the study, “Are there any concerns you would like us to address immediately to better care for you?” Transcribed responses were reviewed, and we calculated the type and frequency of answers.
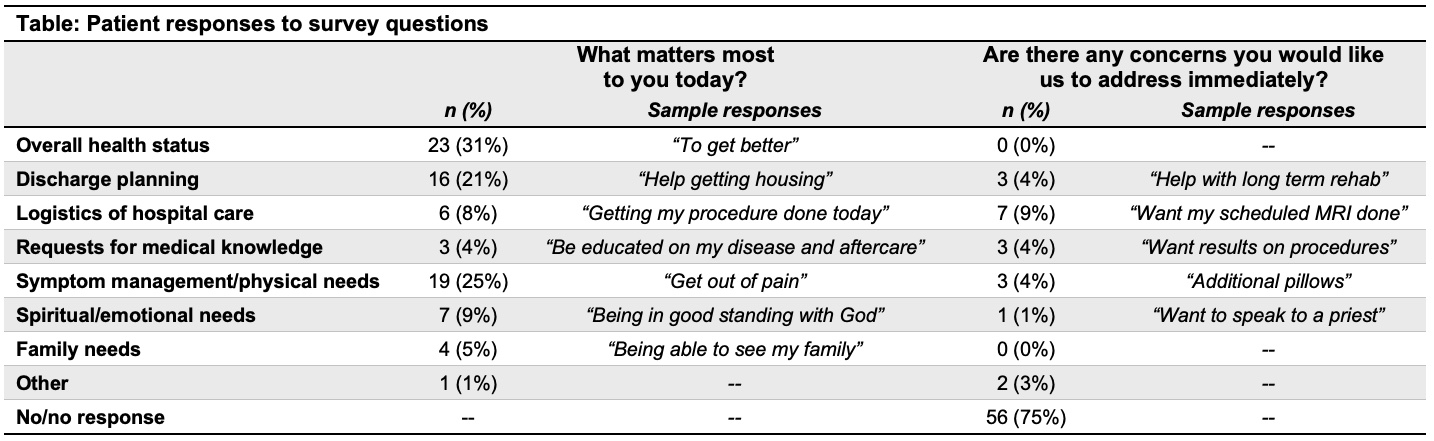
Results: A total of 72 patients were invited to participate, with 66 individuals agreeing to answer the survey questions over 75 individual encounters. The mean age of patients was 58 years (SD = 28), and 38 (58%) patients were male. An interpreter was used in 5 (7%) encounters. We identified the following common categories of responses: overall health status, discharge planning, logistics of hospital care, requests for medical knowledge, symptom management/physical needs, spiritual/emotional needs, and family needs. When asked “what matters most to you today?”, the most common responses related to overall health status (31%, n = 23), symptom management/physical needs (25%, n = 19), and discharge planning (21%, n = 16). Responses included “to heal” (overall health status), “help getting housing” (discharge planning), and “to be warm and comfortable” (symptom management/physical needs). When asked “are there any concerns you would like us to address immediately to better care for you?”, 56 (75%) respondents said “no” or did not answer. The other most common categories were logistics of hospital care (9%, n = 7), followed by discharge planning, symptom management/physical needs, and requests for medical knowledge (all 4%, n = 3). Responses included “get lab work done” (logistics of hospital care), “help with long term rehab” (discharge planning), “additional pillows” (symptom management/physical needs), and “after-surgery instructions [to be] more clear” (requests for medical knowledge) (Table).
Conclusions: Our analysis reveals patients often have a variety of concerns and priorities during their inpatient stay, but that differences in how patients are asked about their priorities can elicit differing answers. Future work into these nuances can help elucidate how better to identify our patients’ priorities and, ultimately, build a framework to consistently address them.