Background: To date, there are limited reports around the use of well-designed information technology tools to enhance throughput communication during interdisciplinary rounds (IDRs). In collaboration with our technology innovations center, we developed a Microsoft Teams IDR tool known as “NORA.” NORA is an automated process-oriented tool designed to extract patient summary information from electronic health record. This platform centralizes substantial amounts of data into a user-friendly interface with convenient remote access capabilities. At our tertiary academic organization, we successfully established NORA as the standard IDR rounding tool across multiple sites and disciplines.
Purpose: Our primary goal was to expand NORA usage to improve our understanding of common barriers that could arise during a planned discharge. Our secondary goal was to compare how these barriers may change over time across different service lines.
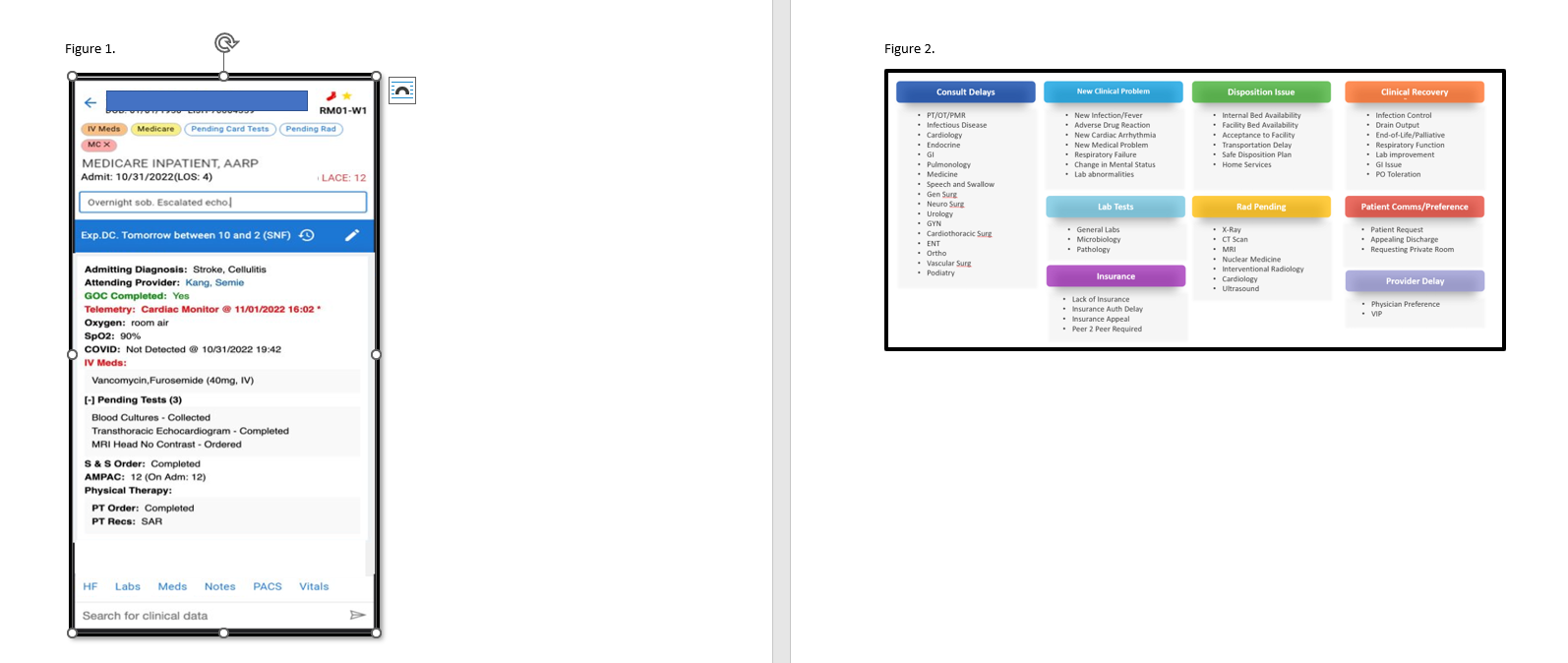
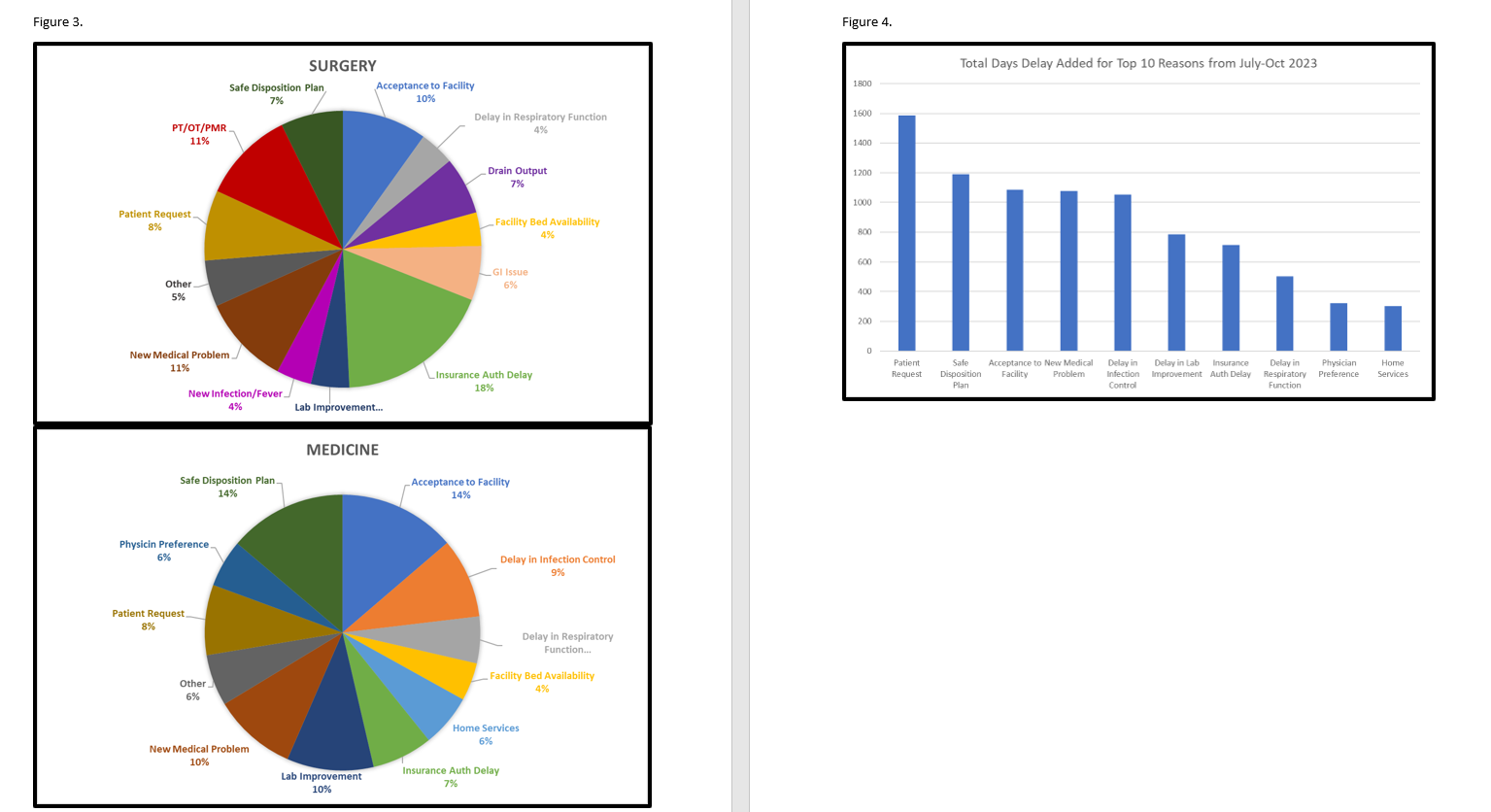
Description: Following the implementation of NORA from 2021 to 2023, our throughput efficiency significantly improved across our sites. Remarkably at one site, we successfully reduced excess days per case to -0.75. Encouraged by this reduction, we expanded NORA across co-managed surgical service lines. The NORA user interface includes active diagnoses, vital signs, medications, laboratory/radiographic results and updated consultant recommendations. The patient summary on NORA also provides insights into potential throughput barriers, anticipated discharge dates and disposition locations (figure 1). This comprehensive information enables the IDR team to swiftly identify the plan of care for each patient without the need to navigate through multiple sections of the EMR. IDR teams use NORA to set anticipated discharge dates as benchmarks for coordinating tasks. If these targets cannot be met, the discharge date is adjusted, and the reason for the delay is documented within NORA. To comprehensively capture the most prevalent reasons for discharge delay, we identified nine main categories (figure 2). Since July 2023 we collected data from both medicine and co-managed surgical service lines, focusing on not only the common delays but also quantifying the additional time each delay contributes to a patient hospital stay (figures 3 and 4). So far, the highest number of excess days at our sites can be attributed to patient requests to stay longer and the coordination of post-acute care services.
Conclusions: Through the implementation of NORA, we demonstrate the significance of developing high-quality information technology tools and data dashboards to comprehend throughput barriers within the hospital. As hospitalists, we lack sufficient tools to quantify the multitude of daily delays. The collected data provided insights, letting us pinpoint departments where discharge processes could be improved and fine-tuned. Additionally, this information revealed the need for earlier communication with our patients regarding their anticipated date of discharge.