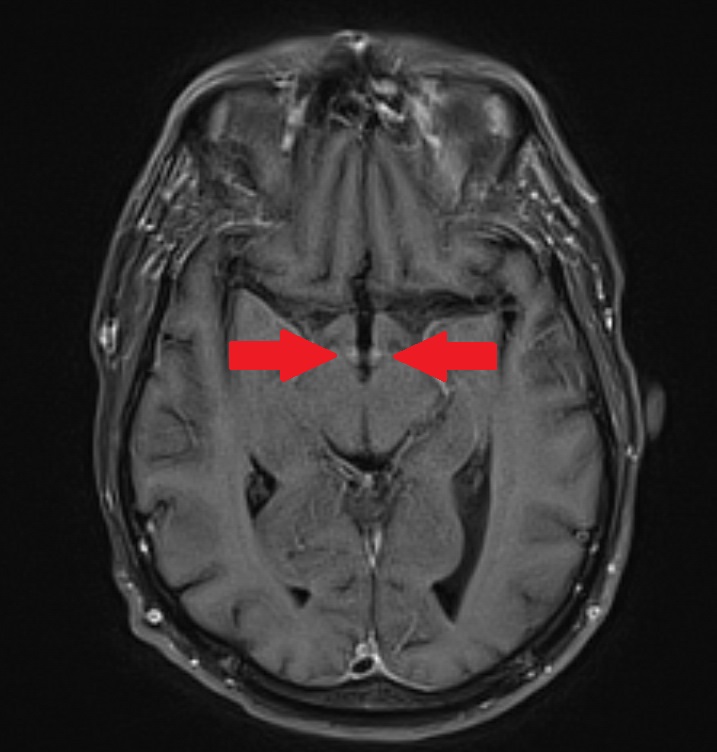
Case Presentation: The patient is an immunosuppressed 57 year old male with small bowel and liver transplant due to trauma from a motor vehicle accident 20 years prior and end ileostomy due to anal carcinoma. His chief complaint was “dizziness,” consisting of lightheadedness and diplopia. His wife described three months of progressive forgetfulness and fabricating stories. He also had parasthesias in his thighs, high ostomy output and progressive exertional dyspnea. On admission, he was well appearing but in mild respiratory distress. Vital signs: BP 106/76, HR 106, RR 24, T 37.0, SpO2 98% on room air. Labs included sodium 130, troponin 14, lactate 6.3, and CRP 7.4. EKG showed sinus tachycardia and non-specific ST changes. CT chest showed small bilateral pleural effusions. The patient was admitted and treated with IV fluids due to suspicion of dehydration from high ostomy output (up to 6L/ day). He remained hypotensive; extensive infection workup was negative. Echocardiogram showed ejection fraction of 30-40% and moderate sized pericardial effusion. Three months prior he had been admitted with a very similar presentation and pattern of lab values (troponin 13, lactate 9). Left heart catheterization showed normal coronary arteries. He was treated for presumed pneumonia and NSTEMI. In the ICU he received high dose thiamine, which is our institution’s standard of care for critically ill patients with altered mental status. He improved and was discharged home. With lack of improvement and review of the prior hospital course, thiamine deficiency was considered. Thiamine level was drawn and empiric treatment was started. MRI brain showed contrast enhancement involving the mammillary bodies and medial anterior thalami with focal area of hemorrhage involving the left mammillary body consistent with Wernicke’s encephalopathy.[1] Thiamine level later returned low (62 nmol/L; normal range 70-180 nmol/L). After five days of high dose IV thiamine, the patient experienced complete resolution of his exertional dyspnea, memory issues, diplopia, and parasthesias. Echocardiogram was repeated and showed normalized EF to 55%. He was discharged with oral and IM thiamine to ensure good effect in case of unreliable absorption. Eighteen days after discharge he was transitioned to oral thiamine with close follow up.
Discussion: Thiamine deficiency causing beriberi is classically associated with alcohol use. However, thiamine deficiency can occur in many clinical situations including alcohol use, malnutrition, malabsorption, loop diuretic use, malignancy, and HIV.[2-6] Here, lactic acid and troponin levels were diagnostic clues. Thiamine pyrophosphate is a crucial co-factor in the citric acid cycle and prevents lactate buildup.[7] A slowed or stopped citric acid cycle damages high energy cells, including myocardial cells, leading to elevated troponins.
Conclusions: Thiamine repletion is considered safe and should be initiated empirically when deficiency is suspected since whole blood testing can take several days.[8] Thiamine administration is therapeutic and diagnostic as ventricular function and lactic acid levels typically normalize quickly with repletion. Providers should consider thiamine deficiency in patients with risk factors as it mimics other disease states.