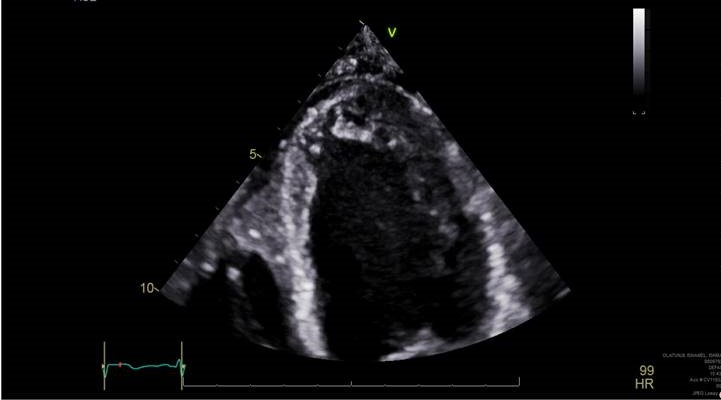
Case Presentation: 24-year-old male with no significant past medical history came to the emergency department (ED) after he was found unconscious at home. He had agonal respirations, which was reversed by Narcan at the scene and the patient was combative in the ED.He was tachycardic with heart rate of 120, saturation maintained at 92% on 15 L of oxygen. Physical examination was unremarkable except for bilateral decreased air entry. His initial blood gas showed a pH of 7.13, PCO2 56, bicarbonate 18, creatinine was 2.5, lactate was 11.6, CPK 13,532, troponin 2.1. Urine drug screen was positive for cocaine and marijuana. Chest x-ray showed patchy pneumonia entire Left lung and right lower lobe which was confirmed by CT chest. Patient was admitted to the ICU, for acute respiratory failure and possible aspiration pneumonia and was treated with vancomycin and Zosyn for 4 days, narrowed down to Augmentin for the next 3 days. Meanwhile patient’s lactate, CPK, creatinine was trending down on adequate hydration and chest x-ray 2 days later, showed interval improvement of pneumonia. On the second day, patient was complaining of sensory motor weakness of right lower extremity,clinical examination showed a sciatic nerve distribution pattern . His troponin trended up from 2.1 to 8.9 ng/ml . Serial EKGs demonstrated sinus tachycardia, however no ischemic changes. Patient was initiated on aspirin and Plavix and IV heparin, however when UDS came back positive for cocaine, heparin was discontinued considering the possibility of type 2 NSTEMI. Echo cardiogram was obtained, which showed normal ejection fraction, but the presence of non-compaction cardiomyopathy. Due to the high risk of arrhythmias and sudden cardiac death associated with non-compaction cardiomyopathy patient was discharged on life vest. The plan is to get a cardiac MRI as outpatient to consider ICD placement.
Discussion: Left ventricular noncompaction (LVNC) was described by Grant in 1926 describes a ventricular wall anatomy characterized by prominent left ventricular (LV) trabeculae, a thin compacted layer, and deep intertrabecular recesses. Clinical presentation can occur at any age, range from asymptomatic to end-stage heart failure, or be associated with lethal arrhythmias, sudden cardiac death, or thromboembolic events.The American Heart Association’s new guidelines on ICD implantation, permit the primary prophylactic implantation of an ICD in patients with NCCM. Long-term oral anticoagulation is indicated in particular for patients with atrial fibrillation, impaired left ventricular function, or demonstrated intracardiac thrombi.
Conclusions: Our patient here was fortunate enough to get an echocardiogram and the condition was diagnosed early enough, as the risk of sudden cardiac death is high with noncompaction cardiomyopathy. Patient’s neuromuscular weakness gradually improved with physical therapy. Because the disease can run in families, the affected patients’ relatives should undergo screening and it is advisable for patients to be examined by a neurologist in order to rule out any accompanying neuromuscular disturbances.