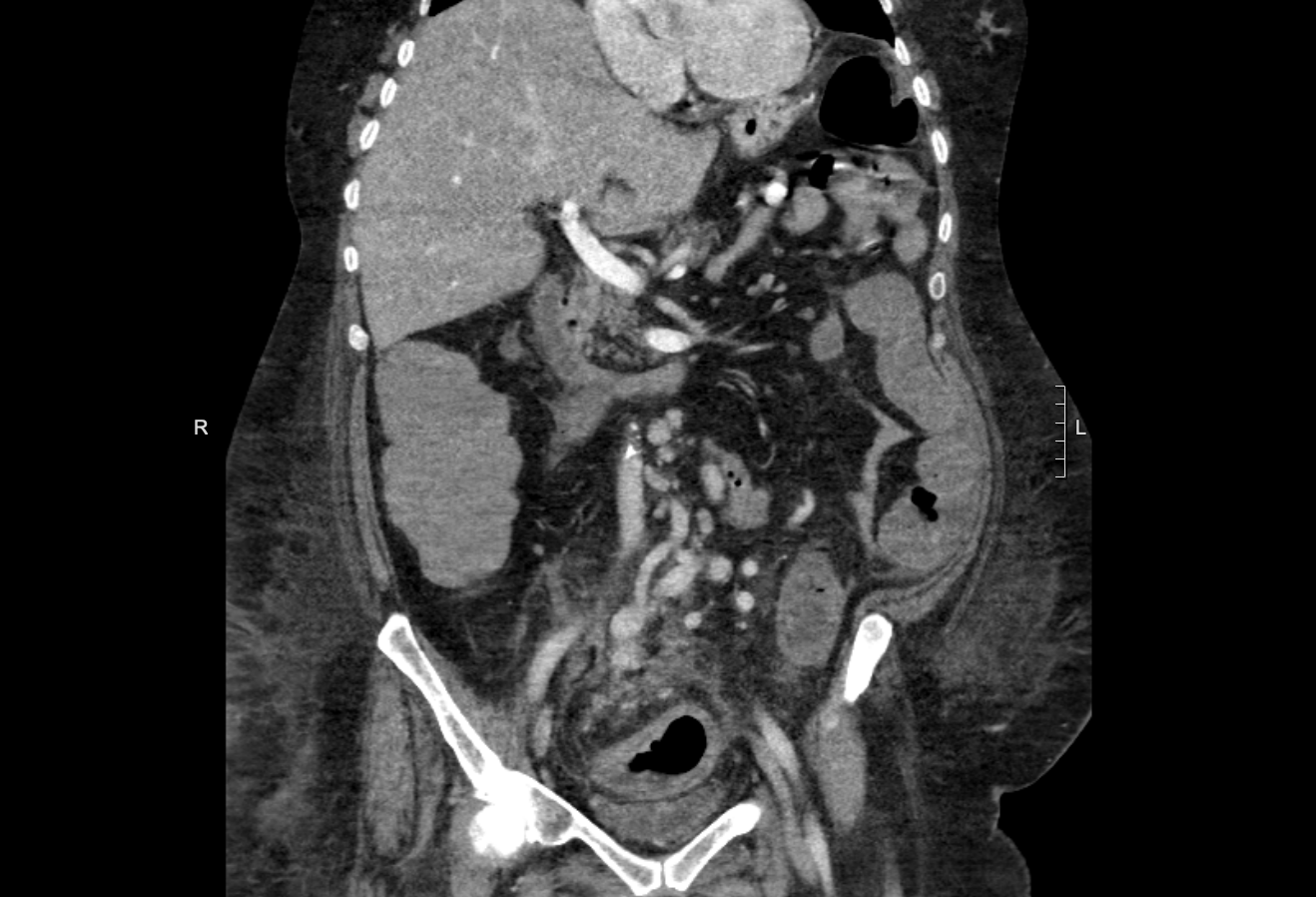
Case Presentation: A 64 year old female with a pmh of Klinefelter’s syndrome (XXY) s/p gender reassignment surgery, hypothyroidism, asthma, obesity, hyperlipidemia and diverticulosis presented with 6 days of worsening lower abdominal pain and discomfort with diarrhea, mucus and bloody stools along with low-grade fevers, nausea, fatigue, weakness and lower abdominal cramping exacerbated by bowel movements. On examination she was febrile, tachycardic, and had tenderness to palpation over bilateral lower quadrants without rebound, rigidity or guarding. Labs showed hyponatremia, hypokalemia, metabolic acidosis, leukocytosis, and mildly elevated lactic acid. CT with IV contrast showed severe proctocolitis. The distribution was similar to ischemic colitis but was considered unlikely, given the avid mesenteric arterial enhancement, colonic mucosal enhancement as well as continued enhancement of the venous vasculature of the pelvis and left lower quadrant. She was admitted with a diagnosis of infectious versus inflammatory colitis and was started on antibiotics. She underwent a colonoscopy which showed that there was diffuse erythema and erosions consistent with significant colitis from the proximal sigmoid colon to the rectum. Pathology report revealed lamina propria congestion, focal hemorrhage and acute inflammation without transmural involvement. The patient was discharged on oral antibiotics. She returned in 2 weeks with worsening symptoms and lab values with severe hyponatremia and leukocytosis and was readmitted. CT with IV contrast again showed colitis of uncertain etiology. But given no definitive diagnosis had been made at this point, a CT Angiogram was obtained and revealed IMA-IMV fistula shunting blood away from the left lateral branch of the IMA. She subsequently underwent embolization of the shunt by IR resulting in good recovery without requiring any bowel resection.
Discussion: Spontaneous IMA to IMV fistula is considered to be extremely rare. Only 33 cases of AVF affecting the inferior mesenteric vessels have ever been described in literature. Of those cases reported, 20 cases were congenital or idiopathic, while the others were secondary to previous operation or trauma.1 AVF causes steal phenomenon which occurs when blood flow is directed away from its intended location by a vessel with less resistance to flow.1 In this patient, the AVF located between the IMA and IMV allowed blood to flow away from the capillary bed of the colon, resulting in ischemia.Symptoms of ischemic colitis vary depending on the severity of vessel occlusion. The classic triad of ischemic colitis includes postprandial pain(out of proportion), fear of eating and involuntary weight loss. Additional symptoms include bloody diarrhea, enteropathic protein loss, sepsis, and symptomatic colonic strictures.5 Not all cases of ischemic colitis are clear. Our patient’s case shared features of both infectious and ischemic colitis. The patient’s elevated leukocyte count and fever and ct with iv contrast showing good venous return led investigators to the diagnosis of infectious versus inflammatory colitis. Inferior mesenteric AVF’s are rare and are treated with resection of the fistula or with embolization of the fistula. Some require subtotal or total colectomy 6. Our patient had good outcome with embolization the AVF.
Conclusions: High suspicion is required when colitis involves any specific arterial territory but has initial normal imaging.AV Fistula can cause misinterpretation as infectious or inflammatory causes.