Background: While understanding the cognitive contributions to diagnosis has become important, few studies have aimed to understand physician diagnostic reasoning in real-time. Using a case-based approach, we sought to: (a) characterize differences in diagnostic reasoning among hospitalists; and (b) identify factors associated with diagnostic accuracy.
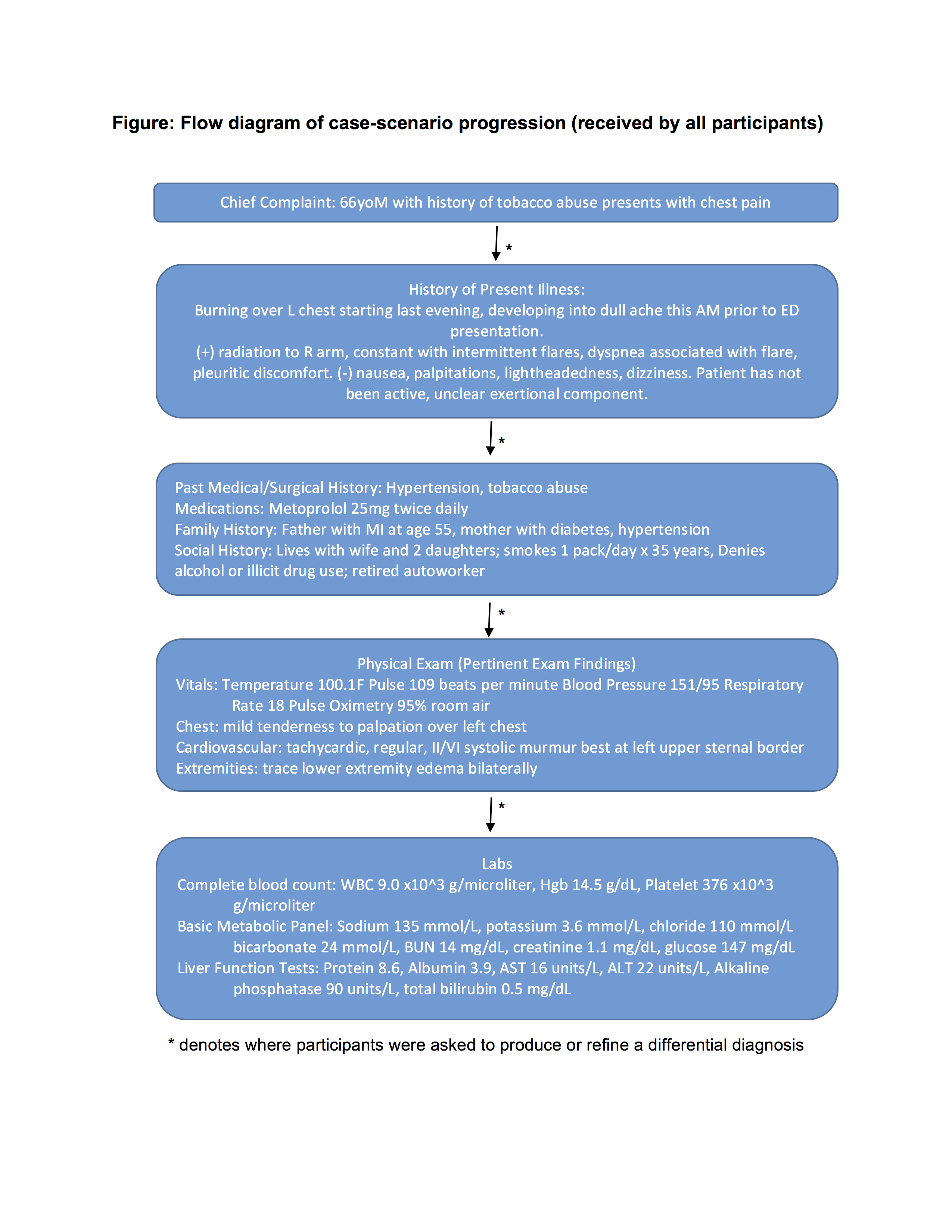
Methods: A total of 10 hospital medicine attending physicians from an academic medical center agreed to take part in the case-based interview. Hospitalists were provided pertinent information regarding a patient’s presentation in a step-wise fashion (Figure), and asked to formulate a differential diagnosis following each new piece of data. Following presentation of basic labs, participants were able to request results for additional lab tests and studies, which were provided if available. An updated clinical course was also provided to participants at regular intervals. All sessions were audio-recorded and transcribed verbatim. Synthesis of quantitative and qualitative data using mixed methods were used to identify key findings by two reviewers (AG, VC).
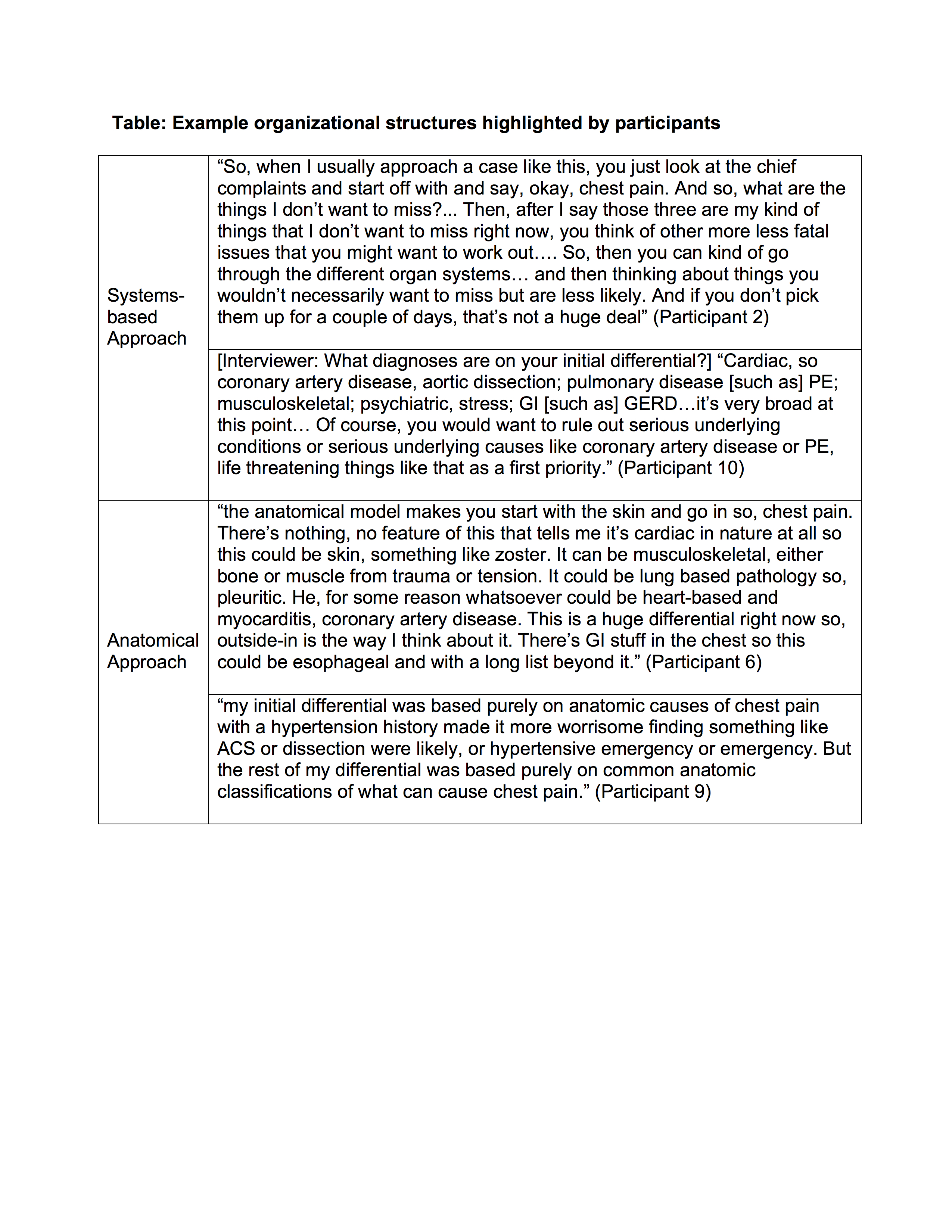
Results: Ten hospitalists (5 male and 5 female) participated in interviews. The average years post-residency was 7.2 (range 2-16 years. The correct diagnosis (shingles) was included in the final differential of 4 of the 10 participants. Hospitalists that identified the correct answer differed from those that did not in several ways. First, they included more diagnoses in their initial differentials (mean 9.75 [range 8-13, SD 1.18] vs 6.0 [range 4.0-10.0, SD 0.89], p=0.03). Second, hospitalists that included the correct diagnosis also used a specific organizational structure to generate candidate diagnoses, including systems-based (i.e., cardiovascular, pulmonary) and anatomical (i.e., chest, abdomen) approaches (Table). Third, while all hospitalists prioritized life-threatening diagnoses, those whose initial differential included only those causes were less likely to arrive at the correct diagnosis and more likely to anchor on these initial diagnoses further into the case. Finally, those correctly identifying the diagnosis frequently re-examined data regarding the patient’s initial presentation or physical examination.
Conclusions: Although limited to a small sample size from one academic medical center, certain behaviors in diagnostic evaluation appear to limit anchoring and improve diagnostic accuracy. Frequent and intentional re-evaluation of data in the context of the patient’s initial presentation may be important in refining differential diagnoses.