Background: Medical housestaff must participate in a handoff process when transitioning between rotations on hospital services. During this time, a new team of residents assumes care for multiple patients. A prior study demonstrated that this critical period of transition is associated with increased mortality among hospitalized patients. Methods of improving daily patient handoffs to overnight housestaff have been widely studied, however, improving handoffs at the end of rotations remains under-investigated. At our large academic medical institution, housestaff are expected to complete written signout on multiple medically complex patients at the end of each rotation. Prior to this intervention, there was no standardized tool to facilitate these handoffs between rotations.
Purpose: The purpose of this study was to investigate the impact of a standardized end-of-rotation handoff template on handoff completeness, resident satisfaction and perceived patient safety.
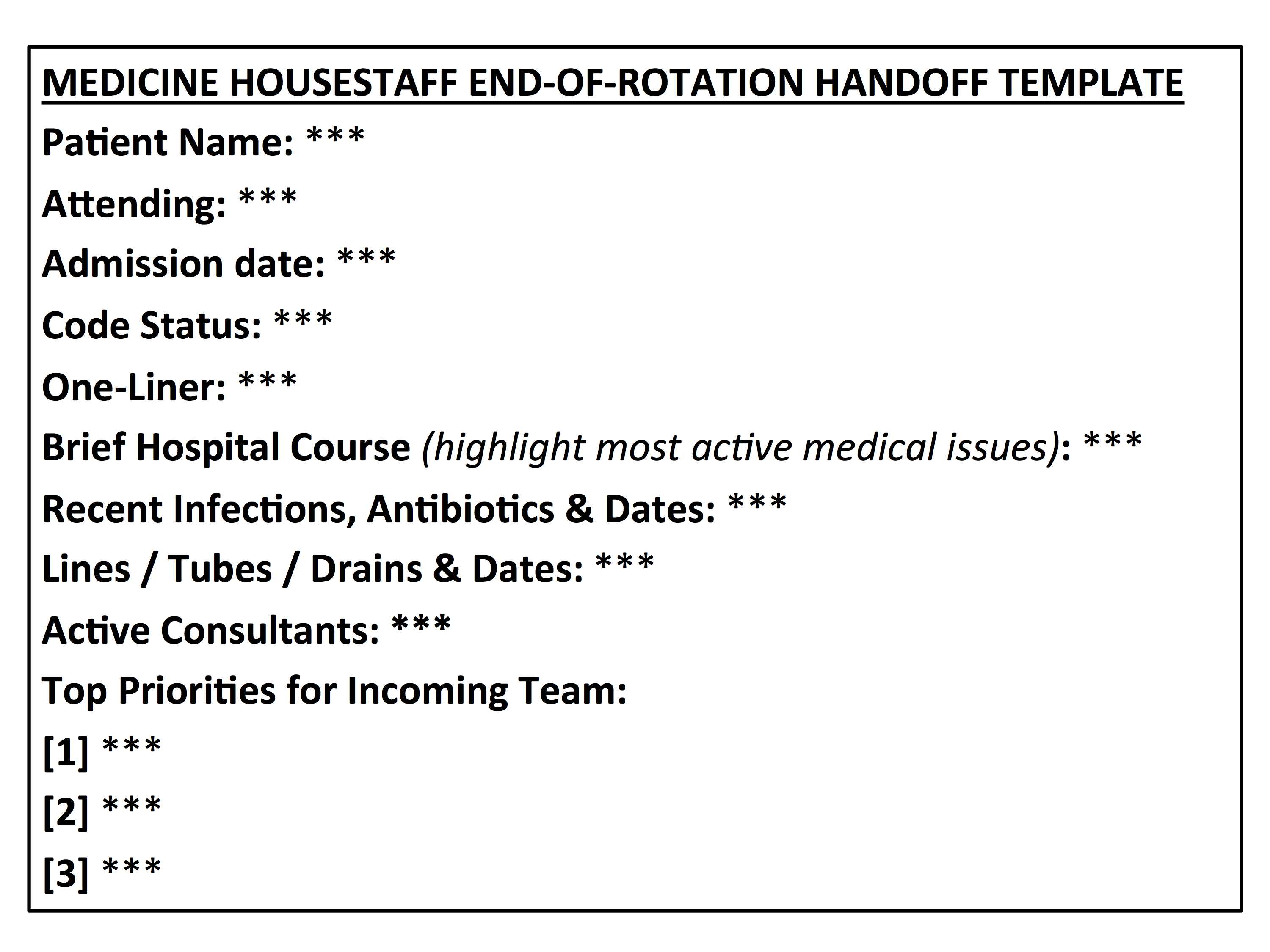
Description: Our study was conducted among internal medicine housestaff from July 2015-November 2017 at a single academic tertiary care center. Baseline data was collected via anonymous surveys to housestaff to assess resident satisfaction with the handoff process, perceived ability for the handoff process to prevent medical errors, and comfort with assuming care of new patients under this process. A standardized handoff template was then created by evaluating written handoffs for deficiencies and incorporating housestaff feedback. Housestaff were asked to use this template for their written signouts at the end of rotations starting July 2016. Follow-up data on resident perception of the handoff process was collected via housestaff surveys in October 2017. Additionally, pre and post-intervention written handoffs were evaluated for completeness using two published grading scales for written handoffs, the “Faculty Checklist” and the “UPDATED Audit Tool,” in which higher scores correlate with more complete written handoffs.
During the study period, 90 handoffs (45 pre-intervention and 45-post intervention) were blinded and audited by two internal medicine residents for completeness. Under the UPDATED Audit Tool, average score for handoff completeness improved from 5.23 to 6.74 (p<0.0001) and under the Faculty Checklist, average score improved from 6.17 to 7.50 (p<0.0001). Resident satisfaction increased from 40% to 92% (p=0.0001) and perceived safety of the handoff process improved from 4% to 46% (p=0.0008). Other significant survey changes included improvements in the perception of receiving a thorough signout (36% to 88%, p=0.0001), providing relevant administrative data (36% to 85%, p=0.0004), receiving a prioritized problem list (20% to 73%, p=0.0002), providing anticipatory guidance (24% to 62%, p=0.0067) and comfort assuming care of patients on the first day of the new block (44% to 96%, p=0.001).
Conclusions: Use of a standardized end-of-rotation handoff template during resident transition periods resulted in increased completeness of handoffs as measured by two published grading scales. Standardization of end-of-rotation handoff templates also resulted in increased resident satisfaction and perceived patient safety.