Background: Sleep deprivation has deleterious effects on immune function, wound healing, insulin resistance, pain, and even mortality. Patients in hospitals often suffer from sleep deprivation due to environmental noise and interruptions from staff. The American Academy of Nursing Choosing Wisely guidelines recommend not to “wake the patient for routine care unless the patient’s condition or care specifically requires it,” however this guideline is often not adhered to.
Purpose: In this quality improvement project we proposed a multifaceted, multipronged intervention to improve the environment and promote sleep.in hospitalized patients.
Description: In a 34-bed acute medicine inpatient unit of an urban, tertiary academic hospital, we utilized a multidisciplinary intervention which included: (1) an education and awareness campaign for day and evening staff through staff meetings and daily huddles, and use of signs and posters, (2) identification of local unit champions from nursing and patient care advocates (PCAs), and (3) delivery of a sleep package that included an eye mask, earplugs, lavender scent pad, and non-caffeinated tea. The sleep package was delivered by PCAs at bedtime with a script asking patients whether they would like the TV turned off, blinds closed, lights off, or anything else to improve sleep. Random patients who received the intervention were given the Richards-Campbell Sleep Questionnaire survey the following morning. The survey asks participants to rate the quality of the previous night’s sleep (1 to 10, with the higher number corresponding to better sleep) through five questions. Additionally, patients’ response to the HCAHPS satisfaction question, “During this hospital stay, how often was the area around your room quiet at night?” was reviewed monthly. Pre-intervention data was collected from January 1, 2017 – June 30, 2017 and compared to post-intervention data collected July 1 – November 13, 2017.
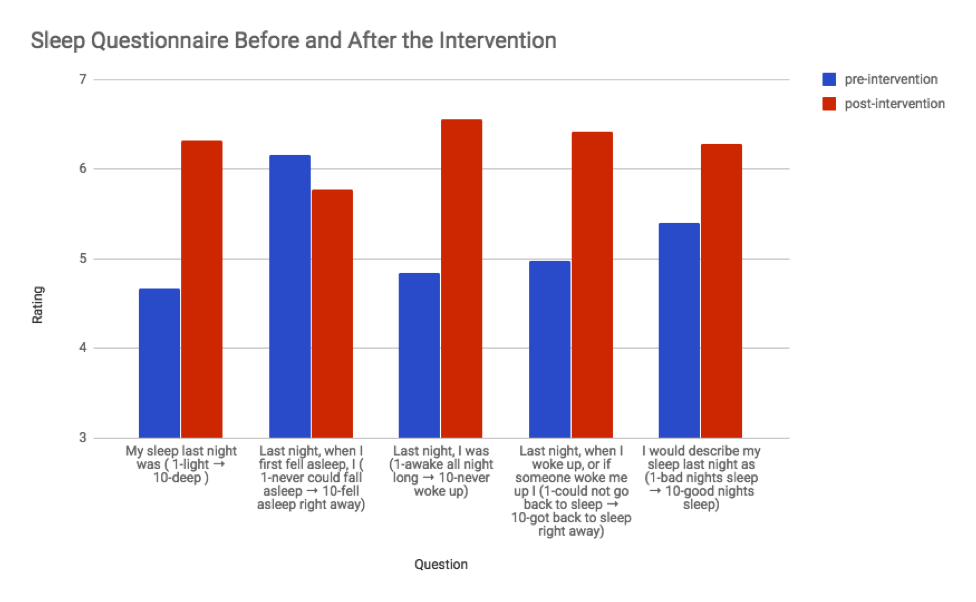
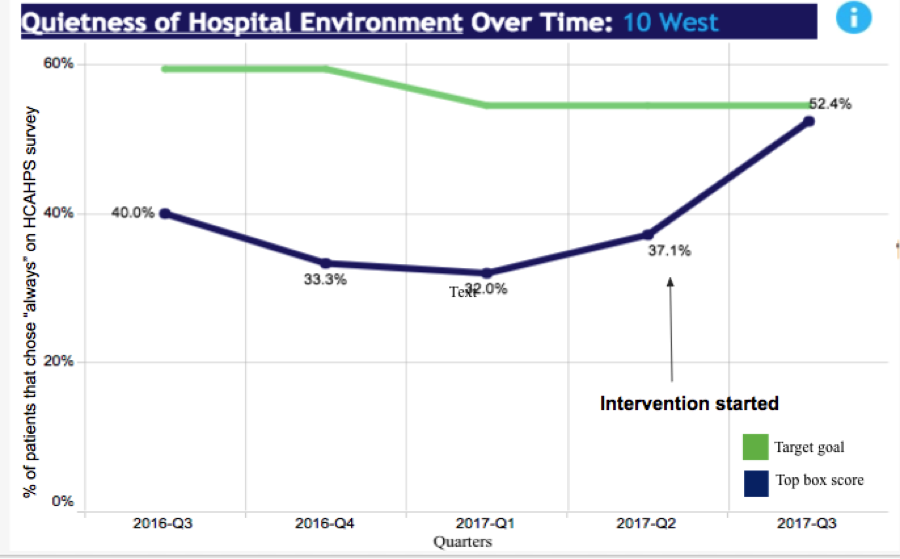
As compared to 49 pre-interventions surveys, scores increased on four of the five questions in 56 post-intervention surveys (question 1, 4.66 vs. 6.32, (p=0.027), question 2, 6.16 vs. 5.78, (p=0.23), question 3, 4.84 vs. 6.55, (p=0.103), question 4, 4.98 vs. 6.41, (p=0.50), question 5, 5.40 vs. 6.27, p=0.314) [See Figure 1]. A 15.3% increase was also noted in patients answering “always” to the HCAHPS question question pertaining to quietness at night in the post-intervention period [See Figure 2].
Conclusions: By implementing this robust, non-pharmacologic, multidisciplinary intervention, ratings on four of the five sleep quality questions on the Richards-Campbell Sleep Questionnaire increased, with one demonstrating statistical significance. Additionally, we noted an increase in the quietness at night HCAHPS question. These results are preliminary, and we will need to demonstrate sustainability with further implementation. This project could serve as a model for other institutions to improve patient experience.