Background: Community acquired severity scores are well known and used routinely in predicting mortality and risk of inpatient and ICU admission in suspected bacterial pneumonia patients. However such scores have not been studied in patients with influenza infection and influenza pneumonia. We attempted to validate one such score, CURB65 and and identify other scores that could improve the prediction in Influenza patients.
Methods: All patients presenting to any of the Henry Ford Health System emergency room sites between December 2016 and April 2017 who had a positive influenza PCR testing were identified. Of the 2842 patients, 1215 were chosen randomly for individual chart analysis. 904 patients were placed in an analysis cohort and 311 patients were placed in a validation cohort. ED arrival data including Uremia (BUN>20), Creatinine, WBC count, Absolute Lymphocyte Count, Hemoglobin, Platelet count, Albumin, Serum blood glucose, pH were collected by chart abstraction. Presenting vital signs such as Fever (temperature >38.3 in first 24 hours), documentation of confusion, tachypnea (respiratory rate >30), hypotension (systolic blood pressure <90 and diastolic <60), presence of pneumonia and pleural effusion on chest xray were also taken for analysis. Outcomes studied were death from any cause within 30 days of presentation, inpatient admission, ICU admission, length of stay more than 48 hours after presentation to ED. Multivariate logistic regression identified presence of confusion, uremia, tachypnea, hypotension, presence of pneumonia on xray, age>65, hypoalbuminemia (uncorrected albumin<3), elevated Creatinine (more than 2) as significant predictors of outcomes studied. Of these we used CURB65, CURP65 (replacing presence of pneumonia for blood pressure) and CURP65-AC (addition of hypoalbuminemia and elevated Creatinine) scores and tested their predictability using ROC curves and sensitivity analysis against the validation cohort.
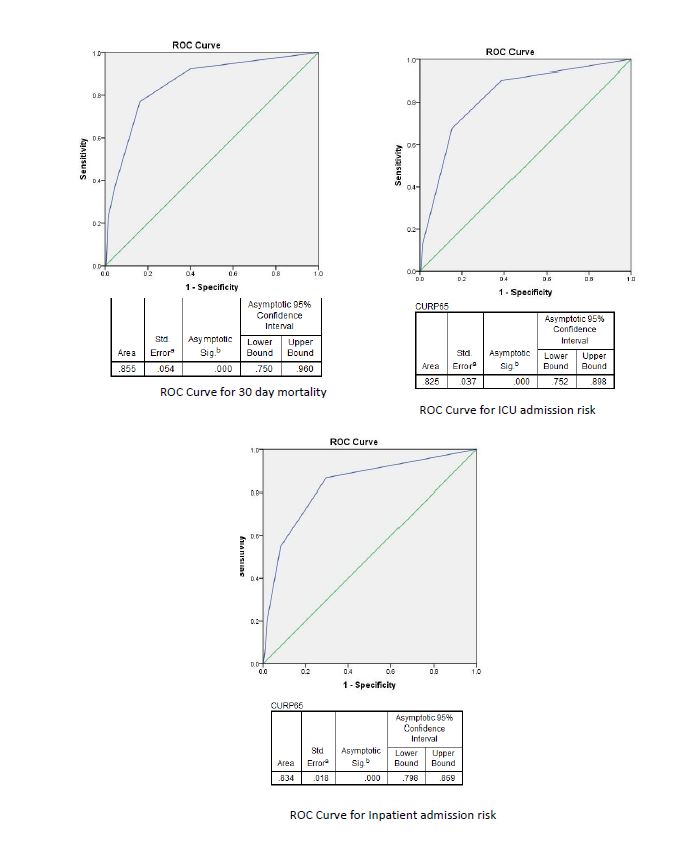
Results: Of the 904 patients analyzed there were 13 mortality events within 30 days. CURB65, CURP65 and CURP65-AC all performed well in predicting the mortality in Influenza patients with a near identical AUC 0.85 (0.75 to 0.96). There were 31 escalation of care to the ICU. CURB65 had an AUC of 0.81, CURP65 AUC was 0.82 CURP-AC had a AUC of 0.82 for ICU patients. CURB65 AUC for inpatient admission was 0.81, CURP65 AUC was 0.83, CURP-AC had the best AUC of 0.85. The prediction capability of these scores was then tested against the validation cohort to determine sensitivity and specificity. CURB65 and CURP65 score of 2 or more predicted mortality with a sensitivity of 100% and specificity of 81%. For ICU admissions CURB65 >1 had a sensitivity of 58% and specificity of 83.2%, CURP65 >1 performed better with sensitivity of 83% and specificity of specificity of 82%. A score of 3 or more increased the specificity of CURB65 to 90% and CURP65 to 95%
Conclusions: From these results it is apparent that using the CURP65 score increases the prediction potential over CURB65 in Influenza pneumonia. CURP65 score may provide additional information to the ED physician or the admitting physician to determine risk of deterioration and aid in disposition decision making. Further studies are needed to determine if this is a good score for 30 day mortality prediction in influenza patients.